Interamerican
Journal of Heath Sciences 4 (2024) - ISSN 2953-3724
DOI:
10.59471/ijhsc2024182
OHVIRA syndrome: report of a case in Bolivia
Síndrome
de OHVIRA: reporte de un caso en Bolivia
Leonel
Rivero Castedo1  , Jhossmar
Cristians Auza-Santivañez2
, Jhossmar
Cristians Auza-Santivañez2  ,
Roberto Carlos Jimenez Fernandez3
,
Roberto Carlos Jimenez Fernandez3  ,
Elier Carrera González4
,
Elier Carrera González4  ,
Alba Rossio López Castillo5
,
Alba Rossio López Castillo5  ,
Jorge Soneira Pérez6
,
Jorge Soneira Pérez6 
1Universidad
Privada Franz Tamayo. Santa Cruz, Bolivia.
2Ministerio
de Salud y Deportes. Instituto Académico Científico Quispe-Cornejo. La Paz, Bolivia.
3Universidad Católica Boliviana “San Pablo”. Santa Cruz, Bolívia.
4Hospital Clínico-Quirúrgico Miguel
Enríquez. Unidad de
cuidados Intensivo. La Habana, Cuba.
5Hospital de San Lorenzo. Tarija, Bolivia.
6Hospital Universitario Clínico
Quirúrgico “Dr. Miguel Enríquez”. La Habana, Cuba.

Received: 20-08-2023 Revised: 15-11-2023
Accepted: 22-02-2024 Published: 23-02-2024
How to Cite: Rivero Castedo L, Auza-Santivañez JC, Jimenez-Fernandez RC,
Carrera González E, López Castillo AR, Soneira Pérez J. OHVIRA syndrome: report of a case
in Bolivia. Interamerican Journal of Health Sciences. 2024;4:182. https://doi.org/10.59471/ijhsc2024182
ABSTRACT
Introduction: the OHVIRA Syndrome was
described by Herlyn Werner Wunderlich and in 1976 Wunderlich described a
grouping of right renal aplasia with bicornuate uterus and simple vagina in the
presence of an isolated hematocervix, as a characteristic triad uterus didelphys,
intercepted hemivagina and ipsilateral renal anomaly, it is generally performed
The diagnosis occurs in puberty at the beginning of menarche, with manifest
symptoms of progressive dysmenorrhea and non-specific abdominal pain in the
hypochondrium; urinary retention, urinary infection or a pelvic mass usually
appear.
Clinical case: the case of a 13 - year -
old patient is presented, who comes to the clinic with abdominal pain and
transvaginal bleeding. Imaging studies are performed and due to the
characteristics of said studies, the presence of OHVIRA Syndrome is suspected.
Discussion. Once the
imaging studies were performed and the diagnosis confirmed, a surgical
procedure was performed under general anesthesia. Through exploratory
laparotomy, a bicornuate uterus was visualized, the right uterus larger than
the left, and adherence to the abdominal wall, so an open intervention was
decided.
Conclusions: OHVIRA syndrome coexists
with a rare malformation and is often misdiagnosed as other more common
etiologies of dysmenorrhea in adolescents, as a consequence it delays a correct
and early diagnosis, increasing the risk of kidney damage and its complications.
In our clinical case, a timely diagnosis was made and surgical treatment was
subsequently planned with a favorable outcome.
KEYWORDS
Dysmenorrhea; Hematometra;
Müllerian Malformations; Renal Agenesis.
RESUMEN
Introducción: el Síndrome de OHVIRA fue descrito
por Herlyn Werner Wunderlich y en 1976 Wunderlich describió una agrupación de
aplasia renal derecha con útero bicorne y vagina simple en presencia de un
hematocérvix aislado, como triada característica útero didelfo, hemivagina
interceptada y anomalía renal ipsilateral, generalmente se realiza el
diagnostico en la pubertad en inicio de la menarca, con clínica manifestada de
dismenorrea progresiva y dolor abdominal no específico en hipocondrio, suele
aparecer retención urinaria, infección urinaria o una masa pélvica.
Caso clínico: se presenta el caso de una paciente
de 13 años de edad, que acude a consulta con dolor abdominal y sangrado
transvaginal, se realiza estudios de imagen y por las características de dichos
estudios se sospecha de la presencia de un Síndrome de OHVIRA.
Discusión: al realizarse los estudios de imagen
y confirmar el diagnóstico se realiza procedimiento quirúrgico bajo anestesia
general, mediante laparotomía exploratoria se visualiza útero bicorne, derecho
mayor tamaño que el izquierdo, adherencia a pared abdominal, por lo que se
decide intervención abierta.
Conclusiones: al síndrome de OHVIRA coexiste una
malformación rara y a menudo se diagnostica equivocadamente como otras
etiologías más comunes de dismenorrea en adolescentes, como consecuencia
retrasa un diagnóstico correcto y temprano, aumentado el riesgo de daño renal y
sus complicaciones. En nuestro caso clínico, se dio un diagnóstico oportuno y
posteriormente se planificó un tratamiento quirúrgico con una evolución
favorable.
PALABRAS CLAVES
Dismenorrea; Hematómetra;
Malformaciones Mullerianas; Agenesia Renal.
INTRODUCTION
OHVIRA syndrome was described in 1925 by Herlyn Werner Wunderlich, (1)
according to Zhu et al. He relates that it was initially described in 1971 by
Herlyn-Werner, (2) and in 1976 Wunderlich described a grouping of
right renal aplasia with the bicornuate uterus and simple vagina in the
presence of an isolated hematocrit (3) as a characteristic triad
didelphic uterus, intercepted hemivagina and ipsilateral renal anomaly, the
diagnosis is usually made at puberty at the onset of menarche, with clinical
manifestations of progressive dysmenorrhea and non-specific abdominal pain in
the hypochondrium, urinary retention, urinary tract infection or a pelvic mass.
The incidence of this pathology is estimated at 0.1 to 3.8 %, (4)
representing 0.16-10 % of all mullerian malformations (occurring in 1/2,000 to
1/28. 000 women), the etiology is usually unknown, but it can be originated by
the unprecedented development of the Müllerian and Wolffian ducts,(5) around
the eighth week of gestation,(6) the Müllerian or paramesonephric
ducts fuse forming the uterus, the proximal two thirds of the female organ and
the cervix with a central septum, which begins to be reabsorbed at nine weeks
and finally leaves a single cavity, depending on the height of the defect, the
duplicity in the HWWS ends at the uterine or cervical level, or reaches lower,
having a duplex vagina, the incidence of ipsilateral anomaly is 100 %, this is
due to the interaction relationship between the paramesonephric and mesonephric
ducts during renal development, (6) it is a challenge the early
diagnosis, besides it is not usually a single presentation, renal agenesis can
be accompanied by other ipsilateral renal anomalies, (7) ectopic
ureter, ureterocele and vesicoureteral reflux (VUR), contralateral urological
anomalies such as VUR, mega ureter and dysplastic kidney, (6) in
addition to clinical hematocolpos, irregular menstruation, such as severe
dysmenorrhea or amenorrhea. Another variant is cervical atresia and a double
cervix with hemicervical obstruction with a rudimentary hemiuterus; in a large
percentage of OHVIRA syndrome, the septum is thick and limits the distension of
the hemivagina, resulting in retrograde bleeding causing endometriosis. (7)
In patients with OHVIRA syndrome, ovarian function is not
compromised, and reproductive condition is affected by problems such as
endometriosis, obstructed hemiuterus pregnancies, development of pelvic
abscesses, and abdominal wall adhesions have been described.
We present the case of a 13-year-old female patient who comes to the
clinic with abdominal pain and transvaginal bleeding. Imaging studies are
performed, and due to the characteristics of these studies, the presence of
OHVIRA syndrome is suspected.
CLINICAL CASE
A female patient of 13 years of age comes to consultation with a
clinical picture of abdominal pain and transvaginal bleeding to the anamnesis
refers to not remembering the date of last menstruation FUM (irregular
menstruation), physical examination at the abdominal level is evident infra
umbilical middle scar and drainage points in surgical points Mc Burney, this as
background one year ago of an exploratory laparotomy, also refers intervention
with uterine drainage, aspiration for biopsy of both uterus and
permeabilization of the cervix. Gestations: 0, Abortions: 0, Births: 0, flat
abdomen, positive hydrothermal sounds (+), painful to superficial and deep
palpation in hypogastrium, both iliac fossae, normal external genitalia, no
evidence of transvaginal bleeding and no cervix palpation; with negative pack
test, normal hemogram, normal blood chemistry and normal cuagulogram,
fibrinogen 310mg/dL (200 - 400 mg/dL), factor O Rh+, negative CRP, normal
general urine test, negative urine culture.
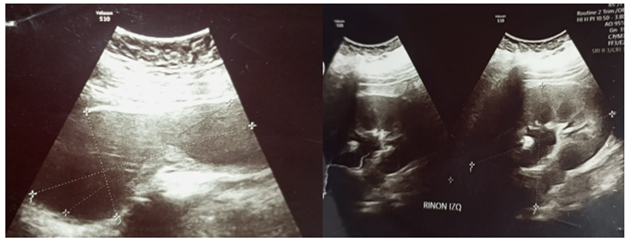
A gynecological ultrasound was performed to be compatible with
hematometra (Vol. 291.44). Abdominal ultrasound showed two solid masses in the
pelvic excavation area, one measuring (7.6 x 5.8 x 5.8 x 5.6 cm) and the other
(8.7 x 5.9 x 5.5 cm), both joined in a flange, with no endometrial image
observed, the right kidney was absent, left kidney measured 11.2 x 8.2 cm,
slight pyelocaliceal dilatation is observe (Figure 1A- 1B).
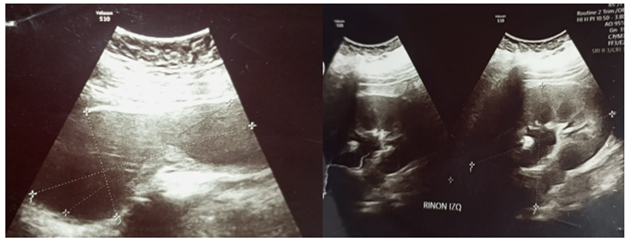
Figura 1. A: Ecografía ginecológica, evidencia
imagen econegaticas compatible con hematómetra, dos masas sólidas, ambas se
unen por una brida, miometrio homogéneo, útero en anteroversoflexión, útero
didelfo, saco de Douglas libre. B: Ecografía abdominal, que evidencia presencia de riñón
izquierdo y dilatación de los calices menores en forma moderada, agenesia renal
derecha
In the abdominal and pelvis tomography without contrast, the left
kidney was observed at the abdominal level, right renal agenesis, adjacent to
it, there was a nodular image of 14 mm, with a spleen attenuation coefficient
of 42UH; at the pelvis level, there was a preserved bladder, a didelphic uterus
associated with hematometra, the other organs were preserved. In addition,
urotomography is performed where the previous conclusion is confirmed,
obtaining the measures of the left kidney of 12.8 cm longitudinal, 72 cm
transverse, 69 cm anteroposterior, and 69 cm anteroposterior.
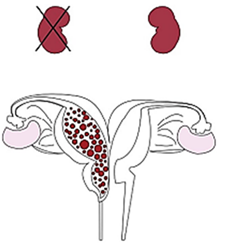
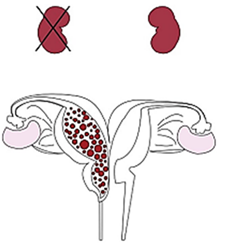
Figure 2. Graphic representation of
the triad of OHVIRA syndrome (hemivaginal obstruction and ipsilateral renal
impairment), of the reported case
Medical conduct
After performing imaging studies and confirming the diagnosis, a
surgical procedure was performed under general anesthesia by exploratory
laparotomy; a bicornuate uterus was visualized, the right larger than the left
(+/- 4 cm), adherence to the abdominal wall, so it was decided to perform open
surgery. The urology service team intervened with cystoscopy and placement of a
double “J” catheter in the left kidney, with fluoroscopy control, the catheter
was in good position, and a Foley catheter N°16 Fr was placed; Then an
infraumbilical median incision is made with excision of anterior scarring, in
the abdominal cavity multiple adhesions are visualized to the anterior wall and
anterior face of the uterus, visualizing two uteri, the right one of greater
size, with multiple adhesions that make it impossible to see the fallopian
tubes, if the right ovary is visualized, the left uterus of smaller size (+/- 5
x 4cm) which is attached at the bottom of the larger uterus, with free and
visible tubes and ovaries, vertical hysterotomy is performed (+/- 6cm),
entering the uterine cavity, obtaining dense liquid, dark color, not fetid,
which is aspirated and digital exploration is performed, where there is no
evidence of communication to the left uterine sketch, but no duct was excavated
towards the cervical orifice, with obstruction in the lower part of the cervix,
in the exploration by vaginal canal, suprapubic valva is placed, channeling and
forming new cervix and communication with the uterine cavity, then endotracheal
tube N°8 is introduced into the uterine cavity, through the cervical canal,
passing through the vaginal canal until it reaches the external part, where it
is fixed on the inner side of the left thigh, all adhesions are removed,
hysterorrhaphy is performed, empirical broad-spectrum antibiotic therapy is
indicated, the management of this patient was multidisciplinary.
DISCUSSION
The classification of OHVIRA syndrome is by clinical features in
complete or incomplete obstruction of the hemivagina, as follows:
Classification 1, patients with complete obstruction of the hemivagina, and
classification 2, patients with partially obstructed hemivagina. In the
follow-up of the patients in a period of 1 to 120 months, the median was 17
months; renal agenesis favored the right side, all patients underwent resection
of the vaginal septum and drainage of the hematocolpos, some women were married
and sexually active, 85 % of the women who decided to conceive became pregnant,
the pregnancy occurred in a higher percentage in the uterus contralateral to
the hemivaginal septum, other women experienced separate pregnancies in each of
the bilateral uteri, in this group there were no pathological pregnancies or
pregnancy complications.(2)
The classification of Mullerian anomalies, according to Velandia et
al., had improved since 1979 when they were described by Buttiram and
Gibbonsen, the AFS (American et al.) published a classification that was used
for decades, and in 2004, Acien and co-authors generated a system based on the
embryological origin of the malformations, considering the pathophysiology and
the various related organs in the development of the female genital system,
different from them Oppelt P and participants describe the VCUAAM system
(Vagina et al. Associated Malformation), integrating findings found in the
vagina, cervix, uterus, and adnexa, and the associated anomalies were assigned
to a group M, relative to each specific group. However, it was observed that
several congenital malformations were not contained in the important categories
or subcategories of this system.
For example, the cervical septate uterus with or without a vaginal
septum, the didelphic uterus with an obstructive vaginal septum, and the
bicornuate uterus with cervical or vaginal aplasia. This is why the European
Society of Human Reproduction and Embryology (ESHRE) and the European Society
of Gynaecological Endoscopy (ESGE) developed a new system established under the
name CONUTA (Congenital et al.), which is based on the morphology of the female
genital tract, embryological origin as the main class, cervical and vaginal
anomalies are classified in independent subclasses, with clinical disposition
being the main initial site to make a good diagnosis and to establish treatment
with alternatives, however the arcuate uterus is excluded from this classification.
· Using the tables to make the diagnosis, the challenge of which
method to use continues, based on ultrasound, invasive methods, and others
based on high-quality images, sensitivity, and specificity; their
contraindications and limitations for each patient must be taken into account.
The determination of OHVIRA syndrome is mainly based on
the following complementary examinations:
·
Pelvic ultrasound: It is the first line of
diagnostic imaging. It allows for identifying uterine anomalies, detecting
partial vaginal obstruction by the vaginal septum, and evaluating the kidneys.
It has a sensitivity of 78-90 % for OHVIRA, with a 92,1 % of use. (8)
·
Renal ultrasound: Evaluates the presence or
absence of ipsilateral kidney. It is useful since 50 % of OHVIRA is associated
with renal agenesis.
·
Magnetic resonance imaging (MRI): Gold standard
for soft tissue resolution. It may be evidence of the obstructive origin of
hematocolpos. Sensitivity >95 %. With 74,6 % of use. (8)
·
Voiding cystourethrography is the gold standard
for ruling out vesicoureteral reflux of the ipsilateral kidney.
·
Urotomography provides detailed 3D images of the
urinary tract, with lower sensitivity to detect low-grade reflux, and is
usually more expensive, with less exposure to radiation.
·
Laparoscopy: In ambiguous cases, it allows for
the visualization and corroboration of uterine and tubal anomalies.
·
Biopsy: Histological analysis of the vaginal
septum to rule out other causes of obstruction.
There are risks before surgery of making an incomplete incision and
presenting the need for a new surgery, in addition to predisposing to
endometriosis and complications in case of pregnancy that may occur in patients
with OHVIRA syndrome previously corrected surgically include
Spontaneous abortion, preterm labor (associated with increased uterine
contractions and premature cervical changes, the rate can be as high as 50 %),
Restricted intrauterine growth (due to uterine vascular anomalies leading to
placental insufficiency), abnormal fetal presentation, preeclampsia, postpartum
hemorrhage (due to uterine hypotonia or placental retention due to anatomical
abnormalities), infertility (due to recurrent synechiae or tubal blockages
after corrective surgery), uterine rupture (very rare, but possible due to
weakness of the muscular wall), renal complications (impaired renal function in
pregnancy), it is recommended not to consume NSAIDs. Preconception counseling
and close prenatal controls are recommended in the future, being essential for
the early detection and timely management of these potential obstetric
complications.(7) According to Candiani et al. (9), more
than 85 % of the patients who sought pregnancy were successful, as is the case
of Reis et al. (10)
Similar clinical cases were reported in other countries, as in the
case of Kueppers et al. (6) using the VCUAM classification and the
specific classification elaborated by Zhu et al., with one case being
“Classification 1” “Subclass 1. 1”, due to acute clinical presentation,
avoiding complications that can evolve rapidly; with ‘Classification 2’ there
is a post-puberty clinical presentation, presenting years after menarche. (6)
We must consider differential diagnoses in neonates, such as embryonic
rhabdomyosarcoma (botryoid sarcoma), ureteral prolapse, hymenal or vaginal
cysts (Gartner), prolapsed ectopic ureterocele, hydometrocolpos.(6,11)
It is important to avoid complications due to hemivaginal
obstruction, which is an indication for surgery and drainage of the
hydrocolloids after the operation, to monitor for possible recurrent
obstruction of the hemivagina due to renal anomalies, particularly in patients
under five years of age. (6) Chan et al. report the case of fetal
autopsy, giving OHVIRA results, which was performed on the fetus born dead in
the third trimester, revealed a didelphic uterus, obstructed left hemivagina
and a left pelvic atrophic duplex kidney, with left ureters entering obstructed
left hemivagina, associated with anorectal malformation, a single right
umbilical artery and spina bifida occulta.(12) The literature also
describes OHVIRA syndrome in its late presentation in a 14-year-old adolescent
with a rare variant of this syndrome; the authors highlight the relatively long
delay in diagnosis two years after menarche, attributed to the presence of a
contralateral non-obstructive hemivagina that allowed a partial menstrual flow,(9,13)
which in some cases the relative management and Antibiotic therapy.(14)
The diagnosis was made by abdominal ultrasound and confirmed by abdominal and
pelvic tomography and urotomography. The medical treatment administered in the
case was micronized progesterone 200 mg daily dose case scheduled surgery, as
in most cases.(2) As we can see, the conduct has been the same in
most reports; the diagnosis was by ultrasonography, urotomography, and magnetic
resonance imaging, being the gold standard, and the definitive management was
corrective surgery.
CONCLUSIONS
OHVIRA syndrome coexists with a rare malformation and is often
misdiagnosed as other more common etiologies of dysmenorrhea in adolescents; as
a consequence, it delays a correct and early diagnosis, increasing the risk of
renal damage and its complications.
In our clinical case, a timely diagnosis was made, and subsequently,
surgical treatment was planned with a favorable evolution. We consider that
knowledge of the pathophysiological characteristics, clinical presentation, and
diagnosis is the best tool for the timely medical-surgical therapeutic
management of these patients and to avoid their suffering from complications.
REFERENCES
1. Paz-Montañez JJ,
Gaitán-Guzmán LF, Acosta-Aragón MA. Síndrome de OHVIRA, a propósito de un caso.
Universidad y Salud. [Internet]. 2020; 22(3): 288–291.
Disponible en: https://doi.org/10.22267/rus.202203.201
2. Herlyn U, Werner H.
Simultaneous occurrence of an open Gartner-duct cyst, a homolateral aplasia of
the kidney and a double uterus as a typical syndrome of abnormalities). Journal
Geburtshilfe und Frauenheilkunde. [Internet]. 1971; Vol. 31. Available at: https://pubmed.ncbi.nlm.nih.gov/5573697/
3. Wunderlich M. Unusual
form of genital malformation with aplasia of the right kidney. Zentralblatt Fur
Gynakologie. 1976; 98(9): 559–562. Available at: https://pubmed.ncbi.nlm.nih.gov/936822/
4. Velandia-Avendaño MC,
Sepúlveda-Agudelo J. Revisión de la clasificación y diagnóstico de
malformaciones mullerianas. Revista Médicas UIS. 2018; 31(2): 57–63. Disponible
en: https://doi.org/10.18273/revmed.v31n2-2018007
5. Han BH, Park SB, Lee YJ, Lee KS, Lee YK. Uterus didelphys with blind hemivagina and ipsilateral renal
agenesis (Herlyn-Werner-Wunderlich syndrome) suspected on the presence of
hydrocolpos on prenatal sonography. Journal of Clinical Ultrasound. 2013;
41(6): 380–382. Available at: https://doi.org/10.1002/jcu.21950
6. Zhu L, Chen N, Tong JL,
Wang W, Zhang L, Lang JH. New Classification of Herlyn-Werner-Wunderlich
Syndrome. Chinese Medical Journal. [Internet]. 2015; 128(2): 222–225. Available
at: https://doi.org/10.4103/0366-6999.149208
7. Kueppers J, Wehrli L,
Zundel S, Shavit S, Stahr N, Szavay PO. OHVIRA-syndrome in a newborn. Journal
of Pediatric Surgery Case Reports. [Internet]. 2021; 69, 101859. Available at:
https://doi.org/10.1016/j.epsc.2021.101859
8. Reis M, Vicente A,
Cominho J, Gomes A, Martins L, Nunes F. Pyometra and Pregnancy with
Herlyn-Werner-Wunderlich Syndrome. Revista Brasileira de
Ginecologia e Obstetrícia / RBGO Gynecology and Obstetrics. [Internet]. 2016; 38(12): 623–628. Disponible en: https://doi.org/10.1055/s-0036-1594304
9. Candiani M, Vercellini
P, Ferrero-Caroggio C, Fedele F, Salvatore S, Fedele L. Conservative treatment
of Herlyn-Werner-Wunderlich syndrome: Analysis and long-term follow-up of 51
cases. European Journal of Obstetrics & Gynecology and Reproductive Biology.
[Internet]. 2022; 275: 84–90. Available at: https://doi.org/10.1016/j.ejogrb.2022.06.0134
10. Elgohary MA, Naik R,
Elkafafi M, Hamed H, Ali Y. Obstructed hemivagina and ipsilateral renal anomaly
(OHVIRA) syndrome: A case report. Journal of Pediatric Surgery Case Reports.
[Internet]. 2023; 95, 102662. Available at: https://doi.org/10.1016/j.epsc.2023.102662
11. Chan ES, Stefanovici C.
Obstructed Hemivagina and Ipsilateral Renal Anomaly (OHVIRA) - A Fetal Autopsy
Case. Journal of Pediatric and Adolescent Gynecology: [Internet]. 2022; 35(5):
593–596. Available at: https://doi.org/10.1016/j.jpag.2022.02.003
12. Yung SSF, Ngu S, Cheung
VYT. Late presentation of a variant of Herlyn–Werner–Wunderlich syndrome.
International Journal of Gynecology & Obstetrics. [Internet]. 2016; 133(2):
238–239. Available at: https://doi.org/10.1016/j.ijgo.2015.10.006
13. Figueroa-Blanco AF,
Montañez-Aldana MÁ. Herlyn-Werner-Wünderlinch syndrome: case report. Case Reports. [Internet]. 2018; 4(2): 111–117. Disponible en: https://doi.org/10.15446/cr.v4n2.69279
14. Gutiérrez-Montufar
OO, Zambrano-Moncayo CP, Otálora-Gallego MC, Meneses-Parra AL, Díaz-Yamal I.
Síndrome de Herlyn-Werner-Wunderlich: reporte de caso y revisión de la
literatura. Revista Colombiana de Obstetricia y Ginecología. [Internet]. 2021;
72(4): 407–422. Available at: https://doi.org/10.18597/rcog.3699
CONSENT
The patient's consent
was obtained for this work.
FINANCING
The authors did not receive funding
for the implementation of this study.
CONFLICT OF INTEREST
The authors declare that there is no
conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Leonel Rivero Castedo.
Research: Jhossmar Cristians
Auza-Santiváñez, Leonel Rivero Castedo.
Methodology: Jhossmar Cristians
Auza-Santiváñez, Leonel Rivero Castedo.
Visualization: Roberto Carlos Jiménez
Fernández, Jorge Soneira Pérez, Elier Carrera González.
Original draft: Leonel Rivero Castedo, Jhossmar Cristians Auza-Santivañez, Roberto
Carlos Jimenez-Fernandez, Elier Carrera González, Alba Rossio López Castillo, Jorge
Soneira Pérez.
Writing-revising and editing: Leonel
Rivero Castedo, Jhossmar
Cristians Auza-Santivañez, Roberto Carlos Jimenez-Fernandez, Elier Carrera
González, Alba Rossio López Castillo, Jorge Soneira Pérez.
 , Jhossmar
Cristians Auza-Santivañez2
, Jhossmar
Cristians Auza-Santivañez2  ,
Roberto Carlos Jimenez Fernandez3
,
Roberto Carlos Jimenez Fernandez3  ,
Elier Carrera González4
,
Elier Carrera González4  ,
Alba Rossio López Castillo5
,
Alba Rossio López Castillo5  ,
Jorge Soneira Pérez6
,
Jorge Soneira Pérez6 
![]()