Nursing care for a patient with twin pregnancy and preeclampsia from the Gynecology Service of a clinic in Lima
Cuidados de enfermería a paciente con gestación gemelar y preeclampsia del Servicio de Ginecología de una clínica de Lima
Salazar A Josselyn-Andrea1, Salcedo Victcely-DelCarmen1, Sofía D. Vivanco-Hilario1, Wilter C. Morales-García1
1Unidad de Posgrado de Ciencias de la Salud. Universidad Peruana Unión, Escuela de Posgrado. Lima, Perú.
![]()
Received: 25-06-2023 Revised: 04-09-2023 Accepted: 06-01-2024 Published: 07-01-2024
How to Cite: Josselyn-Andrea SA, Victcely-DelCarmen S, Vivanco-Hilario SD, Morales-García WC. Nursing care for a patient with twin pregnancy and preeclampsia from the Gynecology Service of a clinic in Lima. Interamerican Journal of Health Sciences. 2024; 4:170. https://doi.org/10.59471/ijhsc2024170
ABSTRACT
Preeclampsia is a public health problem and one of the main causes of maternal and perinatal morbidity and mortality, manifested by hypertensive disorders in pregnancy, early diagnosis is essential to reduce complications. With the objective of describing the nursing care in a patient with twin pregnancy and preeclampsia from the gynecology service of a clinic in Lima. The study was carried out with a qualitative approach, single case type, applying the nursing care process (PAE), the assessment guide of the 11 functional patterns of Marjory Gordon in a 33-year-old patient with a 30-year-old twin gestation was used as an instrument. weeks and with preeclampsia. In the results, eight altered functional patterns were identified, prioritizing the sexuality/reproduction pattern: Risk of alteration of the maternal-fetal dyad as evidenced by inadequate prenatal care associated with pregnancy complications. The applied interventions were effective, appreciating the decrease in the risks of preeclampsia; however, faced with the problem of complication of the prenatal period: Risk of malignant hypertension related to pregnancy, the clinical manifestations were stabilized. In conclusion, it was possible to identify the clinical characteristics of the patient with a twin pregnancy with preeclampsia, as well as the identification and description of the risk factors, which allowed highlighting the importance of nursing care, through the development of a care plan. individualized nursing care to reduce complications in the maternal-fetal dyad, framed in the nursing process that identified problems and risks of complications, and at the same time, allowed timely and quality care to be provided.
KEYWORDS
Nursing Care, Twin Gestation, Preeclampsia.
RESUMEN
La preeclampsia es un problema de salud pública y una de las principales causas de morbimortalidad materno y perinatal, manifestada por trastornos hipertensivos en el embarazo, es elemental el diagnostico precoz, para disminuir las complicaciones. El objetivo es describir los cuidados de enfermería en paciente con gestación gemelar y preeclampsia del servicio de ginecología de una clínica de Lima. El estudio se realizó con enfoque cualitativo, tipo caso único, aplicando el proceso de atención de enfermería (PAE), utilizándose como instrumento la guía de valoración de los 11 patrones funcionales de Marjory Gordon en paciente de 33 años, con gestación gemelar de 30 semanas y con preeclampsia. En los resultados se identificaron ocho patrones funcionales alterados, priorizándose el patrón sexualidad/reproducción: Riesgo de alteración de la díada materno-fetal como se evidencia con los cuidados prenatales inadecuados asociado a complicaciones del embarazo. Las intervenciones aplicadas fueron efectivas, apreciando la disminución de riesgos de la preeclampsia; sin embargo, frente al problema de complicación del periodo prenatal: Riesgo de hipertensión maligna relacionado con el embarazo, se lograron estabilizar las manifestaciones clínicas. En conclusion se logró identificar las características clínicas de la paciente con gestación gemelar con preeclampsia y se identificaron y describieron los factores de riesgo, lo que permitió resaltar la importancia de la atención de enfermería, a través de la elaboración de un plan de cuidados individualizado para reducir complicaciones en la díada materno-fetal, enmarcado en el proceso enfermero que identificó problemas y riesgos de complicación, y, permitió brindar cuidados oportunos y de calidad.
PALABRAS CLAVE
Cuidado de Enfermería, Gestación Gemelar, Preeclampsia.
INTRODUCTION
Currently, hypertensive disorders in pregnancy present a high risk of morbidity and mortality for the mother and fetus, so it is necessary to diagnose early in order to achieve better control and limitation of complications (Salas et al., 2020).
In Peru, preeclampsia accounts for 3 % to 22 % of maternal and perinatal deaths, which makes it the second leading cause of maternal death nationally with 32 %, and it is the leading cause at the National Maternal Perinatal Institute of Lima with 43 %. Likewise, between 2012 and 2018, said health institution reported as the first cause of maternal morbidity hypertensive disorders of pregnancy, including preeclampsia with severity criteria, HELLP syndrome, and eclampsia, with 56,6 %(Guevara Ríos, 2019).
The Delgado Clinic, in the period 2014 - 2019, reported 14682 patients seen on an outpatient basis with a diagnosis of essential (primary) hypertension (Delgado Clinic, 2019).
Within the background of said pathology, Bravo et al. (2021) conducted the study entitled “Nursing care plan in preeclampsia. A case report”, concluding that preeclampsia continues to be one of the main causes of maternal morbimortality, which can be detected with good prenatal care, blood pressure control, and pregnancy control as prevention tools.
De La Puente Vaca (2021), in her publication entitled “Importance of Nursing Care in Preeclampsia”, concluded that nursing professionals should provide care that includes psychological, social, and physical aspects, encouraging dialogue and active listening to capture the perceptions and needs of each woman in her disease process.
Preeclampsia is a pregnancy-induced hypertensive pathology with multisystemic involvement that usually occurs after 20 weeks of pregnancy (T. Dulay, 2020).
The pathophysiology is still unknown. However, they state that during pregnancy, the spiral arteries, responsible for placental perfusion, suffer alterations, resulting in low vascular resistance and high tension, altering the endothelial tissue, followed by vascular dysfunction and consequently multiorgan damage, thus originating arterial hypertension, consequently proteinuria, edema, headache, risk of seizures, visual disturbances, epigastralgia, and intrauterine growth restriction (Pereira et al., 2020).
At present, termination/culmination of pregnancy by the most appropriate route is the ideal and conclusive treatment for preeclampsia. However, as long as the clinical criteria of severity indicating termination of pregnancy are not met, preeclampsia will be managed with expectant management (Guevara Ríos, 2019).
Nursing care in the care of the patient with preeclampsia is based on the execution of the scientific method that allows the nursing professional to address potential and actual problems in a comprehensive, logical, and structured manner, comprising the 5 phases: assessment, diagnosis, planning, execution, and evaluation (Salas et al., 2020).
The performance of the nursing activities is based on the scientific methodology of the nursing care process because it allows us to execute the interventions for the achievement of the proposed objectives in order to preserve the hemodynamic stability of the patient in her critical health situation. The prioritization of activities determined the corrective management of hypertension episodes and the prevention of maternal-fetal complication risks in a timely manner, with quality and efficacy (Blanco et al., 2021).
It is important to highlight the linkage of the research with the present case study because it allows the development of an individualized care plan for the care of the patient with twin gestation of 30 weeks with a diagnosis of preeclampsia, hospitalized in the gynecology service. The application of the prioritized care was effective, achieving stabilization of maternal-fetal hemodynamic function and avoiding complications that could put her life at risk.
As a whole, the aim is to strengthen the nursing intervention through effective care, with quality standards to meet the identified needs through effective care, with quality standards for satisfaction of the identified needs, and rescue the human, spiritual, and transpersonal aspects of the patient.
This work was made with the aim to describe nursing care in patients with twin gestation and preeclampsia.
Specific Objectives
To identify the clinical characteristics of the patient with twin gestation and preeclampsia. To identify and describe the risk factors of the patient with twin gestation and preeclampsia. To highlight the importance of nursing care in twin gestation and preeclampsia and to reduce complications. Elaborate a nursing care plan in twin gestation and preeclampsia, using NANDA taxonomy, NOC, NIC, and Lynda Juall Carpenito’s manual of collaborative problems.
Preeclampsia
Preeclampsia is new-onset hypertension or worsening of pre-existing hypertension with proteinuria after 20 weeks of gestation (T.Dulay, 2020). It is a hypertensive disorder that can occur during pregnancy and postpartum and has repercussions on both the mother and the fetus (PAHO, 2019). It becomes a serious condition of pregnancy and represents a major danger as many of its signs are often not evident (Preeclampsia Foundation, 2021).
Causes and risk factors.
There is a wide range of conditions that reflect the complexity of the pathological process, classifying them in terms of:
Family factors: women with maternal and paternal history of arterial hypertension or diabetes, age, and race (Villarreal et al., 2020).
Body mass index and height: Elevated BMI is an important risk factor for preeclampsia (Guevara Rios, 2019).
Pre-existing medical conditions: Diabetes before gestation or others. Number of gestations: Women who have never gestated have a higher risk of developing preeclampsia. Intergestational interval: Women with prolonged intergestational interval may be causative for the development of preeclampsia (Rojas et al., 2019).
History of preeclampsia, use of assisted reproductive technology, infections during pregnancy, paternal factors, and maternal habits are also part of the classification of risk factors (Mayo Clinic, 2022).
Pathophysiology of preeclampsia
Preeclampsia is a disease that occurs only during or after pregnancy and is caused by activation of the vascular endothelium, probably caused by placental ischemia, caused by a defect in the trophoblastic invasion of the uterine spiral arteries. Genetic, immunological, and biochemical causes are mentioned to explain this defect in trophoblast implantation with associated placental ischemia. Due to the activation of the endothelium, various chemical mediators are released, which, by their action, affect the functioning of all organs and systems, causing syndromes associated with preeclampsia (Velumani et al., 2022).
Several factors are involved, the most important of which is the establishment of placental insufficiency, which is responsible for the induction of an antiangiogenic state in the pregnant woman and the development of endothelial dysfunction in various organs that triggers the clinical manifestations of the disease (Guevara Ríos, 2019).
Classification of preeclampsia.
Preeclampsia without severity criteria: This is one with only hypertension greater than or equal to 140/90 mmHg but less than 160/110 mmHg, without hematological, renal, hepatic, pulmonary, or neurological dysfunction, and without evidence of fetal damage (Velumani et al., 2022).
Preeclampsia with severity criteria: Preeclampsia evolves into severe complications such as acute pulmonary edema, renal failure, hypertensive encephalopathy with cerebral hemorrhage, retinal detachment, premature placental abruption, hepatic subcapsular hematoma or hepatic rupture, HELLP syndrome, and death in the pregnant woman, fetus or newborn (Guevara Ríos, 2019).
Clinical manifestations of preeclampsia.
Preeclampsia Foundation (2021) exposes the following clinical manifestations:
Arterial hypertension is one of the main clinical manifestations; proteinuria occurs when proteins come out of the blood and are poured into the urine, edema which comes to be the accumulation of excess fluids, sudden weight gain between 900 grams or more in a week, nausea and vomiting, abdominal pain (stomach area) and shoulder pain are also mentioned.
Also, other literature mentions back pain, headache, visual disturbances, hyperreflexia, increased heart rate, confusion, increased anxiety, shortness of breath, or chest pain; when any of these abnormal symptoms appear for the first time, it may indicate blood pressure or for extreme cases the accumulation of fluid in the lungs (pulmonary edema) (Velumani et al., 2022).
Management of preeclampsia.
The management of preeclampsia begins with the evaluation of the health status of the pregnant woman and the fetus, performing a clinical evaluation of the neurological, respiratory, cardiovascular, hematological, biochemical, and renal functions, as well as an evaluation of fetal well-being with electronic fetal monitoring, biophysical profile and Doppler study of the umbilical and uterine arteries. Pregnant women with preeclampsia, in most cases, require hospitalization for adequate treatment of hypertension, prevention of seizures, optimization of intravascular volume, maintenance of adequate arterial oxygenation, and early detection and treatment of complications (Department of Obstetrics, UC of Chile, 2020).
Management of preeclampsia without severity criteria.
Relative rest, normocaloric, normoproteic and normosodic diet is recommended.
Do not use antihypertensive drugs. The definitive treatment for preeclampsia is termination of pregnancy. If the pregnant woman is 37 weeks or more, the pregnancy should be terminated by vaginal delivery or cesarean section. If the woman is less than 37 weeks and there is no maternal or fetal compromise, management over time is possible, continue with general measures and closely monitor the mother and fetus. If, despite treatment, hypertension is not controlled or if the disease progresses to severe preeclampsia, or if there is preeclampsia or signs of fetal, hematologic, or renal distress, hepatic, pulmonary, or neurologic dysfunction, the pregnancy should be terminated immediately, regardless of gestational age (Guzman et al., 2018).
Management of preeclampsia with severe criteria.
Preeclampsia with severe criteria will progress to severe complications such as acute pulmonary edema, renal failure, hypertensive encephalopathy with cerebral hemorrhage, retinal detachment, placental abruption, subcapsular hematoma, or rupture of the liver, HELLP syndrome, which can lead to death of the pregnant woman, fetus or infant.
Therefore, management should be timely, multidisciplinary, and effective. A pregnant woman who presents vaginal bleeding and signs of placental abruption always suspects preeclampsia as a background condition (Velumani et at., 2022).
In preeclampsia, there is a contraction of the intravascular contents, unlike the usual hypervolemia of the pregnant woman; there is a tendency to oliguria due to lack of fluids despite edema (Tacuri et al., 2022).
Adequate intravascular expansion with 0,9 %saline should be ensured, in case oliguria persists, initiated, followed by a diuretic such as furosemide in order to achieve normalization of blood pressure more quickly and reduce the need for antihypertensive therapy (Rojas et al., 2019).
Strict water balance and monitoring of vital functions should be performed every 15 minutes. Initiate by venous route an infusion of magnesium sulfate for seizure prevention; this solution should be with the initial attack dose, and it is suggested to maintain the infusion for 24 hours after delivery. The administration of magnesium sulfate should be suspended if tendon areflexia or depression of the state of consciousness is detected, and calcium gluconate should be administered in this case. Antihypertensive treatment should only be used if systolic blood pressure is ≥ 160 mmHg or if diastolic blood pressure is ≥ 110 mmHg, in which case the following drugs are recommended: Labetalol, Hydralazine, Methyldopa, Nifedipine (Calderon et al., 2023).
Nursing role
Primary nursing care includes continuous assessment and early identification of signs of worsening disease. Complying with the medical guideline: adequate expansion of the endovascular line with 0,9 %saline solution, 50-60 drops/min for the first liter should be ensured; and, if oliguria persists, the attending physician will prescribe 500 ml of colloid solution on a rapid drip, followed by 10 mg of intravenous furosemide.
Diuresis should be monitored with a bladder catheter connected to a urine collection bag. Blood pressure, heart rate, respiratory rate, and oxygen saturation should be monitored every 15 minutes (Gaona, 2021).
Start an intravenous infusion of magnesium sulfate. The infusion solution is prepared by combining 5 ampoules of 20 % magnesium sulfate (10 ml ampoules) with 50 ml of 0,9 %saline. This solution provides 1 g of magnesium sulfate per 10 ml, and it is recommended to administer 4 grams (40 ml) for 15-20 days as an initial loading dose; continuous infusion of 1 g every hour (10 ml per hour) and maintenance infusion for 24 hours after delivery. When using magnesium sulfate, knee reflex, respiratory rate, which should be at least 14 breaths per minute, and urine output, no less than 25-30 ml/hour, should be monitored (Gaona, 2021).
It is also recommended to monitor O2 saturation with pulse oximetry. The administration of magnesium sulfate should be suspended if tendon hyporeflexia is detected, if there is alteration of consciousness or if there is a tendency to superficial or slow ventilation. In this case, the treating physician will prescribe calcium gluconate, 1 to 2 grams intravenously. Antihypertensive treatment should only be used if the systolic blood pressure is ≥ 160 mmHg or if the diastolic blood pressure is ≥ 110 mmHg (Gaona, 2021).
Risk of alteration of the maternal-fetal dyad.
Vulnerable to disruption of the symbiotic relationship between mother and fetus due to pregnancy-related comorbidities or conditions, which may affect health (Heather Herdman et al., 2021).
Risk factors for the risk of maternal-fetal dyad disruption.
Some of the risk factors are pregnancy complications such as multiple pregnancies, threatened miscarriage, oligohydramnios, and hemorrhage in the second and third half of pregnancy. Other risk factors that can be mentioned are drug dependency, non-compliance with medical indications, inadequate prenatal care, physical abuse, and diabetes, among others (Chesya et al., 2019).
Another source mentions another important risk factor, the compromise of fetal oxygen transport (oligohydramnios, preeclampsia/eclampsia) (Sacks et al., 2020).
Gestational hypertension
Gestational hypertension is high blood pressure during pregnancy. It occurs in approximately 3 out of every 50 pregnancies. This condition is different from chronic hypertension, preeclampsia, and eclampsia. It is a blood pressure problem during pregnancy that begins in the second half of pregnancy and usually disappears after birth (Perez et al., 2019).
Pathophysiology of gestational hypertension.
It is caused by rapid and severe elevation of blood pressure that produces two.
Events: Systemic endothelial dysfunction causing decreased synthesis of vasodilator agents (nitric oxide and prostacyclins) and increased synthesis of cytokines and
vasodilator agents (nitric oxide and prostacyclins) and increased synthesis of cytokines and cell adhesion molecules. In the microcirculation it further increases blood pressure and damages the vascular endothelium, causing fibrinoid necrosis and endothelial proliferation; it also causes peripheral tissue ischemia in target organs. The second affects the renin-angiotensin-aldosterone system by salt concentration and plasma osmolarity, which increases sodium excretion by the kidney, causing intravascular volume deficit (hypovolemia) that affects blood flow and causes terminal organ dysfunction (Perez et al., 2019).
Risk of gestational hypertension
Risks for gestational hypertension include high blood pressure before or during a previous pregnancy, kidney disease, diabetes, under 20 or over 40, and multiple pregnancies (Mayo Clinic, 2022).
Symptoms of gestational hypertension.
The most frequently reported symptoms are High blood pressure during the second half of pregnancy, headache, edema, weight gain, blurred or double vision, nausea or vomiting, abdominal pain, and pollakiuria, as also less prevalent symptoms are dizziness, conjunctival hemorrhage, tinnitus, and epistaxis (Stanford medicine children’s health, 2022).
Complications of gestational hypertension.
The constant evaluation of pregnant patients with hypertensive disorders should be taken into account in order to avoid complications such as Compromised blood vessels, liver failure, renal failure, seizures, placental abruption, insufficient fetal growth, stillbirth, and maternal death (Velumani et al., 2022).
Treatment of gestational hypertension.
The objective is to achieve blood pressure lowering without compromising perfusion of target organs, hemodynamic monitoring of the pregnant woman, and rapid venous access for the administration of antihypertensive drugs (alfa methyldopa, hydralazine, and labetalol), considering a systolic blood pressure of 160 and a diastolic blood pressure ≥110 mm Hg with the aim of stabilizing maternal-fetal health (Stanford medicine children’s health, 2022).
Prevention of gestational hypertension.
Early diagnosis and treatment, Periodic prenatal checkups.
Nursing care for pregnant women with hypertension.
Nursing care is the processes that are applied to reduce the complications of maternal and fetal gestational hypertension, in order to preserve gestation. Among the care for gestational hypertension, we can mention: Relative rest, periodic monitoring of BP and fetal well-being, noncaloric, normoproteic, and normosodic diet, pharmacological treatment with labetalol, hydralazine and alpha-methyldopa, termination of gestation, in cases of more than 37 weeks. If the gestational age is less than 34 weeks, the lungs should be matured with corticosteroids the lungs will be matured with corticosteroids. Do not stop the treatment just after delivery but reduce it gradually (Garcia Lopez, 2020).
Theoretical basis of nursing care in patients with preeclampsia.
It is believed that Hildegard E. Peplau’s theoretical proposal aims to highlight the psychological tasks that are developed in the nurse-patient relationship, which depends on the nurse’s ability to perceive and identify the difficulties in her relationship with the patient and her ability to help them to solve problems. Peplau analyzes the four stages of the nurse-patient relationship, and these have been applied to the care of our patients with preeclampsia: Orientation, identification, utilization, and resolution (Machado et al., 2021).
On the other hand, Jean Watson argues that it is necessary to rescue the human, spiritual, and transpersonal aspects of clinical nursing practice, elaborating her theory “Of human care” based on seven basic assumptions. First, care must be effective and interpersonal. Second, caring involves factors that result from meeting human needs. Third, effective care promotes health and personal growth. Fourth, the responses derived from caregiving accept the person not only as he or she is but as the person can become. Fifth, a caring environment offers the development of potential and allows the person to choose the best action at any given time. Sixth, caring is more “health-genetic” than healing, and seventh, the practice of caring is fundamental to nursing. (Gaona Castillo, 2021).
METHODS
The methodological approach of this study is a qualitative analysis; the type of study is a single clinical case, applying the nursing care process (PAE) to respond to the objectives set in the research about the risk factors of the patient with twin gestation, preeclampsia, and gestational hypertension collaborative problem.
33-year-old female patient, with twin gestation of 30 weeks at the last menstrual period, with a medical diagnosis of preeclampsia, presenting fever, headache, pelvic pain, swollen legs, vaginal discharge with bad odor, and presence of blood without clots, vulnerable to present maternal-fetal complications.
The study period was carried out in the gynecology service, attended from September 9 to 16, 2022.
Information analysis procedure
Source of information
The following was used as a data collection instrument:
Reception of verbal information from the patient with initials F.E.H.M., 33 years old. Direct observation of the patient.
Personal interview with the immediate family member (husband): relevant data from the patient’s medical history: Data from the record of the medical evolution, data from the record of the nursing notes, and results of the diagnostic means.
Performance of the physical examination and comparison of data with the assessment charts. Nursing assessment according to Marjory Gordon’s 11 functional patterns.
Bibliographic review of scientific evidence by other authors from the following sources: Science, Direct, Scielo, Scielo, Elsevier, Google Academic, NANDA International 2021-2023, videos through keywords such as nursing care, twin gestation, preeclampsia.
Collection of information
In order to proceed with the data collection, prior authorization was required from the patient and the personnel responsible for the gynecology service of the clinic, guaranteeing the process of protection and confidentiality of the data provided for the study.
It was carried out in 4 phases:
· First phase: reviewing the patient’s clinical history to extract clinical data such as personal history, family history, reason for consultation, results of auxiliary examinations, main medical diagnosis, medical evolution, nursing diagnoses, and the evolution of nursing care.
· Second phase: The nursing assessment was carried out by means of a personal interview, following Marjory Gordon›s 11 functional patterns assessment guide, using the identification and recognition of the main nursing diagnosis for the preparation of an individualized nursing care plan for the case under study.
· Third phase: The patient was followed up twice on her first day of hospitalization in the gynecology department to assess the evolution of the pregnant woman.
· Fourth and last phase: an exhaustive review of the scientific evidence was carried out, setting limits according to date criteria and limiting the search for information from 2019 to the present. Databases were used: Science, Direct, Scielo, Elsevier, Google Academic, NANDA International 2021-2023, and videos through keywords such as Nursing care, twin gestation, and preeclampsia.
Data processing
The processing and analysis of the data was carried out in three moments: First moment: based on the assessment guide of the 11 functional patterns of Marjory Gordon, a reasoning network based on the “AREA Model” was developed by Pesut and Herdman for the selection of the main nursing diagnosis according to the NANDA-I taxonomy 2021-2023.
Developed by Pesut and Herdman for the selection of the main nursing diagnosis according to the NANDA-I taxonomy 2021-2023.
Second moment: After the choice of the DxEP, we proceeded to the establishment of the outcome criteria (NOC) and interventions (NIC) and the selection and prioritization of the nursing activities.
Third moment: After the execution of the programmed nursing activities, we proceeded to the evaluation of the EAP, with the objective of verifying the effectiveness of the interventions carried out in the nursing care plan for a patient with twin gestation, preeclampsia, and a collaborative problem of gestational hypertension.
CLINICAL CASE
A young adult patient with the initials HMFE, female, 33 years old, from the district of Miraflores, with higher university education, business administrator occupation, was admitted to the emergency area, accompanied by her husband for presenting a temperature of 38,7 °C, headache, tinnitus, abdominal pelvic pain, edema of the lower limbs, vaginal discharge without clots with bad odor and blood. On medical evaluation, she was diagnosed with a twin pregnancy of 30 weeks by the date of her last menstrual period and probable preeclampsia. Hospitalized in the gynecology department, she is in absolute rest, in an antalgic position, with permanent monitoring of vital functions and initiation of medical therapy.
Family history
Mother: Cervical cancer and hypertensive.
Father: Diabetic and hypertensive.
Personal background
Drug allergies: NSAIDS
Food allergy: Lactose intolerant, shellfish allergy.
Metals: Denies
Allergic rhinitis: Denies
Bronchial asthma: Denies
Toxic habits
Tobacco: Denies
Alcohol: Denies
Coffee: Denies
Other intoxicants: Denies
Pathological history
Arterial hypertension, diagnosed in her first pregnancy, with regular treatment of methyldopa 250 mg every 8 hours.
Hypothyroidism diagnosed 3 years ago, with regular treatment with levothyroxine 75 mcg every 24 hours.
Gynecological history
Menarche: at age 12.
FUR: 22.03.22
Gestations: 2
Use of contraceptive methods: Denies
History of PCOS/EPI: Yes
Usual medication for her current pregnancy: Gestavit DHA, folic acid.
Epidemiological background
History of STD: Denied TBC
Contact: Denied
Vaccinations in the last year: Covid 19
Occupation: Administrator
Physical activity: Denied.
Surgical history
Uterine curettage (2020)
Colelap Surgery (2018)
Breast Augmentation Surgery (2012)
PO Liposuction (2012)
Current situation
On evaluation, the patient is lucid, oriented in time, space, and person, Glasgow 15 points, responds to all stimuli, is alert, refers to intense headache on a scale of EVA 10/8, ventilating spontaneously at an FIO2: 0,21 %, with pale skin, hydrated skin, and mucous membranes, normal sweating, distended soft abdomen, pregnant uterus. 21 %, with pale skin, hydrated skin and mucous membranes, normal sweating, distended soft abdomen, pregnant uterus, refers to pain in the abdominal-pelvic region in VAS 10/8 points, ambulates with limitation due to some weakness in lower limbs, edema in lower limbs +++, spontaneous bladder and bowel elimination, vaginal discharge with bad odor and evidence of slight bleeding.
Medical diagnosis
Nulliparous second gestation of 30s x LMP, twin pregnancy, biamniotic, high risk of premature delivery, risk of presenting chorioamnionitis, preeclampsia.
Medical Therapeutics.
Soft, low-sodium diet
Absolute rest
Strict water balance
Bleeding control
Monitoring of vital signs every 2 hours
Fetal monitoring every 4 hours
Parenteral hydration of sodium chloride 0,9 %Methyldopa 250 mg orally every 8 hours.
Nifedipine 30 mg/day orally PRN a Blood pressure over 160/100 mmHg,
Gentamicin 320 mg intravenous every 24 hours.
Clindamycin 600 mg intravenous every 8 hours.
Ceftriaxone 2 grams intravenous every 24 hours.
Simethicone 180 mg orally after meals.
Omeprazole 40 mg intravenous every 24 hours.
Paracetamol 1 gram intravenous PRN at a temperature greater than or equal to 38 °C.
Laboratory tests
Leukocytes: 12,440 Cells/uL (Normal Values: 4,500 - 11,000 Cells/uL)
Hematocrit: 33,2 %(Normal Values: 36 - 43 %)
Platelets: 160 000 Cells/uL (Normal Values: 150 000 – 475 000 Cells/uL)
Hemoglobin: 9,8 g/dL (Normal Range: 12 -16 g/dL)
Creatinine: 1,5 mg/dL (Normal values: 0,5 - 0,9 mg/dL)
Urea: 52 mg/dl (Normal values: 17 - 49 mg/dl)
Protein: 8,3 g/dl (Normal range: 6,0 - 8,3 g/dl)
Glycemia: 85 mg/dl (Normal values: 70 - 100 mg/dl)
SARS-CoV-2 ANTIGEN: Negative,
Hepatitis B Australian Antigen (HBsAg): Non reactive.
HIV Ac (HIV 1-2 Antibodies): Non reactive.
Group and Factor: A negative.
NURSING CARE PROCESS
ASSESSMENT
After introducing my patient according to her clinical report, I proceed to assess her according to Marjory Gordon’s Eleven Functional Patterns of Health (PFS) (Gordon, 1999):
Perception Pattern - Health Management
Nulliparous second gestation patient with current twin gestation of 30 weeks, with history of abortion in 2020, with obstetric ultrasound result of placental accretes.
Altered laboratory results:
Leukocytes: 12,440 Cells/uL,
Hematocrit: 33,2 %,
Platelets: 160 000 Cells/uL,
Hemoglobin: 11,8 g/dl,
Creatinine: 1,3 mg/dl,
Urea: 52 mg/dl,
Blood glucose: 83 mg/dl,
SARS-CoV-2 ANTIGEN: Negative,
Hepatitis B Australian Antigen (HBsAg): Nonreactive,
HIV Ac (HIV 1-2 Antibodies): Nonreactive,
Group and Factor: A-
Nutritional - metabolic pattern
Patient febrile (temperature 38,7), with hot skin, pain in the abdomen, weight: 75 kg, height: 168 cm, BMI: 26,6 (overweight), autonomous in her diet,
eats 5 meals a day, has been gaining weight in the last two months. She consumes liquids frequently, 2 ½ liters per day.
She takes additional supplements for her pregnancy: Gestavid DHA 1 tablet orally every 24 hours and folic acid 10 mg orally every 24 hours.
Allergies to seafood, lactose intolerant.
Good swallowing of food. No nausea or vomiting, nor has she presented them in the last few days.
Pale skin, mucous membranes hydrated.
Elimination pattern
No data is evident.
Activity - exercise pattern
Blood pressure: 190/110 mmHg. Heart rate: 105 beats per minute.
Respiratory rate: 22 breaths per minute, SpO2: 99 %. Rhythmic pulse, no heart murmur.
Eupneic at rest. She is intolerant to physical activity due to her condition.
Remains in bed in an antalgic position, mobilized only for physiological elimination.
Patient with limited gestational ambulation and weakness in lower limbs due to edema and pain.
Edemas in both lower limbs ++ ranging from thighs to feet. Carrier of peripheral line N° 20 in the dorsum of the hand of the left upper limb.
Rest - sleep pattern
No data is evidenced.
Cognitive-perceptual pattern
Lucid patient, oriented in time, space, and person.
At the evaluation of the GLASGOW scale of 15 points, the patient responds to all stimuli and is vigilant.
No language, memory, or hearing problems. No cognitive impairment.
She refers to headache and pelvic pain at the assessment of the VAS scale 10/8.
Self-perception - self-concept pattern
The patient presents signs of anxiety, anguish, fear, nervousness, and headache.
She is aware of her current disease, hypertension, and she is aware of the health risks she presents, so she frequently asks for information about her health status and that of her babies.
She feels loved and supported by her husband.
Role pattern - relationships
She is married and currently living with her husband. She receives support from both families.
Sexuality pattern - reproduction
Pregnant with twins at 30 weeks. She had a previous pregnancy 2 years ago, which culminated in a uterine curettage. Planned pregnancy with medical follow-up.
Congestive breasts. Genitalia with vulvar edema, vaginal bleeding without clots 8 hours ago, without bad odor, no loss of amniotic fluid. Blood group and blood factor: A positive.
Adaptation pattern - stress tolerance
The patient and her husband, very distressed, report being very afraid of losing their babies. They are very cooperative with the treatment indicated by the gynecologist and the care plan required.
Values-beliefs pattern
Practicing Catholic.
PRIORITIZED NURSING DIAGNOSES.
Nursing diagnoses were formulated using the NANDA taxonomy (Heather Herdman et al.,2021).
Pattern Perception - Health Management
(00126). Poor knowledge r/c anxiety m/p request for information about their health status.
Definition: Absence of cognitive information related to a specific topic or its acquisition.
Domain 5: Perception/Cognition
Class 4: Cognition.
Nutritional - Metabolic Pattern
(00007). Hyperthermia r/impaired health status m/p temperature 38. 7°C.
Definition: Core body temperature above the normal diurnal range due to failure of thermoregulation.
Domain 11: Safety/protection
Class 6: Thermoregulation Activity-Exercise
Pattern (00204) Ineffective peripheral tissue perfusion r/c hypertension m/p elevated blood pressures (BP: 160/98 mmHg)
Definition: Decreased blood flow to the periphery, which may compromise health.
Domain 4: Activity/rest
Class 4: Cardiovascular/pulmonary responses.
(00303). Risk of falls e/p decreased lower extremity strength due to edema and pain.
Definition: Adult susceptible to experiencing an event that results in inadvertently resting
On the floor, ground, or other lower level, which may compromise health.
Domain 11: Safety/Security.
Class 2: Physical Injury.
Cognitive-Perceptual Pattern
(00132). Acute Pain r/c biological damage agents m/p headache and abdominopelvic Pain.
Definition: Unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage (International Association for the Study of Pain); sudden or slow onset of any intensity from mild to severe with an anticipated or predictable end, and lasting less than 3 months.
Domain 12: Physical comfort
Class 1: Comfort
Pattern Self-Perception - Self-Concept
(00148). Fear r/unfamiliar situation m/p nervousness and fear
Definition: A basic and intense emotional response that is aroused by the detection of an imminent threat, involving an immediate alarm reaction.
Domain 9: Coping/tolerance to stress.
Class 2: Coping response.
Sexuality - Reproduction Pattern
(00209). Risk of disruption of the maternal-fetal dyad e/p complications in pregnancy.
Definition: Vulnerable to disruption of the symbiotic relationship between mother and fetus due to pregnancy-related comorbidities or conditions that may affect health. NANDA-I Taxonomy (Heather Herdman et al.,2021)
Domain 8: Sexuality
Class 3: Reproduction
(00206). Risk of bleeding and complications of pregnancy (Vaginal bleeding).
Definition: Susceptible to a decrease in blood volume, which may compromise health.
Domain 11: Safety/Protection Class 2: Physical Injury
Pattern Adaptation - Stress Tolerance
(00146). Anxiety r/stressors m/p changes in health status.
Definition: An emotional response to a diffuse threat in which the individual anticipates a nonspecific impending danger, catastrophe, or misfortune.
Domain 9: Coping/stress tolerance. Class 2: Coping response.
Prioritized nursing diagnoses
After exposing the different nursing diagnoses that my patient has, I am going to prioritize the main Nursing Diagnosis (DxEp) by means of a clinical reasoning network based on the AREA Model (Pesut & Herman, 1999). The model establishes clinical reasoning networks based on the relationships that are established between a large number of diagnoses, resulting in a of diagnoses resulting in the most accurate and appropriate diagnosis for each clinical case.
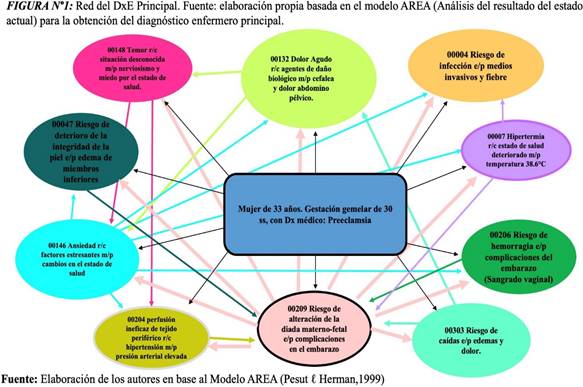
Primary Nursing Diagnosis (DxEp)
After making the interrelation of the diagnoses proposed for the case, we can see in Figure N°1 the choice of the main nursing diagnosis:
(00209). Risk of alteration of the maternal-fetal dyad evidenced by complications in pregnancy due to multiple gestation.
Definition: Vulnerable to disruption of the symbiotic relationship between mother and fetus due to pregnancy-related comorbidities or conditions that may affect health. NANDA-I Taxonomy (Heather Herdman et al.,2021).
Domain 8: Sexuality
Class 3: Reproduction
Nowadays, the probability of a multiple pregnancy has increased considerably due to delayed childbearing and the use of assisted reproductive techniques (Rodrigo et al., 2022).
A multiple pregnancy is considered a risky pregnancy, both for the mother and the fetus, due to the various anatomical and physiological changes that the body undergoes throughout gestation (Stanford Medicine, 2022).
Multiple pregnancies are complicated due to the large volume occupied by the gestation of more than one baby. The uterus bears an excess of weight and can distend, exerting more pressure on the rest of the organs. The placenta grows more than expected, and there is an increase in the mother’s blood hormone levels, concluding that multiple pregnancy places a greater demand on the woman’s body and contribute to an increase in complications such as weight gain, preeclampsia, among other (Mayo Clinic, 2022).
Fetal complications are associated with prematurity and low birth weight since the greater the number of fetuses, the shorter the duration of gestation and the lower the birth weight. Some of the complications include evanescent twin syndrome, feto-fetal transfusion syndrome, congenital disabilities, and growth retardation (Rodrigo et al., 2022).
The maternal-fetal dyad is a bond that is associated with emotional and cognitive aspects that allow the fetus to be recreated as another human being. This bond is expressed through health practices aimed at seeking the protection and well-being of the fetus. As a result of certain problems and complications during pregnancy, such as multiple pregnancies and gestational hypertension, among others, there is a risk of alteration of this bond (Alvarez Martinez, 2021). For this reason, the main nursing diagnosis: (DxEp) was chosen as the Risk of alteration of the maternal-fetal dyad.
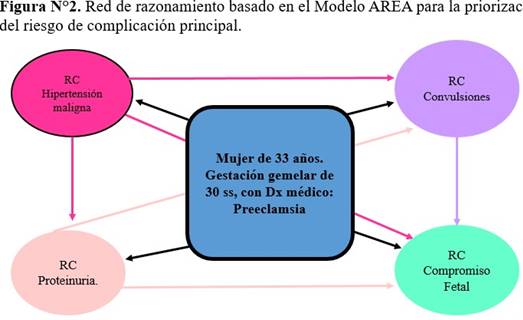
Identification of Collaborative Problems (CP) and their Complication Risks (CR)
To determine the complication problems and complication risks in relation to twin pregnancy with preeclampsia, the Manual of Nursing Diagnoses manual (Carpenito, 2017) was used.
Collaborative Problem in the Prenatal Period: gestational hypertension. The complication risks are:
CR of malignant hypertension, CR of seizures, CR of convulsions.
CR proteinuria
CR of fetal compromise.
Identification of the main CR
Malignant hypertension has been identified as the main complication risk (CR) because it has the highest ratio compared to the others and is associated with CR seizures, CR proteinuria, and CR fetal compromise.
CR Malignant hypertension
Malignant hypertension is very high blood pressure that appears suddenly and rapidly and is capable of triggering serious complications in the patient.
Malignant hypertension is a type of hypertensive emergency, and it is so dangerous that it can cause complications such as organ failure (Medical et al., 2021).
McCarthy (2022) defines malignant hypertension as an increase in blood pressure to such an extent that it causes organ damage, affecting the nervous system, cardiovascular system, and kidneys. It also states that prompt treatment can prevent serious problems such as organ damage to the blood vessels, eyes, heart, spleen, kidneys, and brain.
The role of nursing in severe or malignant hypertension consists of providing absolute rest to the patient, assessing blood pressure frequently, cardiac monitoring, providing reassurance to the patient, and administering oxygen. If necessary, perform an electrocardiogram, monitoring of vital functions, as indicated by the physician, oncolysis, and extraction of analytical tests, and monitoring for possible side effects of drug treatment such as hypotension, nausea, vomiting, and headache. Observe the cardiac monitor for possible rhythm disturbances or signs of myocardial ischemia. Constantly assess the state of consciousness and observe the patient for signs of cerebral hemorrhage (Ybarra et al., 2021).
In conclusion, the clinical manifestation of the patient’s response to the symptomatology of malignant hypertension and the risk of suffering multisystemic organ failure if not controlled, timely intervention should prevent, treat, and control the warning signs of hypertension.
Planning of the main nursing diagnosis (DxEp).
After performing the assessment and obtaining a nursing diagnosis, a follow-up plan is made for the patient using the Nursing Outcomes Classification NOC (Sue Moorhead et al., 2018) and Nursing Interventions Classification NIC (Butcher Howard et al., 2018).
(00209). Risk of alteration of the maternal-fetal dyad evidenced by complications in pregnancy due to multiple gestation.
Definition: Vulnerable to disruption of the symbiotic relationship between mother and fetus due to comorbidities or pregnancy-related conditions that may affect health. NANDA-I Taxonomy (Heather Herdman et al.,2021).
Domain 8: Sexuality
Class 3: Reproduction
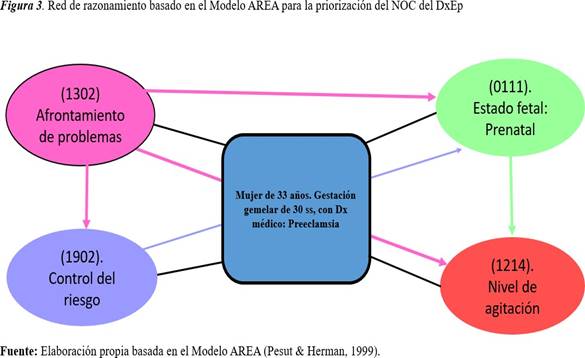
NOC results of the DxEp.
According to the NOC taxonomy, the following corresponds to DxEp:
(0111). Fetal status: Prenatal.
Definition: The degree to which fetal signs are within normal limits from conception to the onset of labor.
Domain: Functional health (1) Class: development and growth (B) (1902). Risk management.
Definition: Personal actions to understand, avoid, eliminate, or reduce modifiable health threats.
Domain: Health knowledge and behavior (IV) Class: Risk control and safety. (T)
(1214). Level of agitation.
Definition: Severity of manifestations of physiological and behavioral stress disorders or biochemical triggers.
Domain: Psychosocial health (III)
Class: Psychological well-being
(1302) Coping with problems.
Definition: Personal actions to manage stressors that strain the individual›s resources.
Domain: Psychosocial health (III)
Class: Psychosocial adaptation (N)
DxEp NOC Prioritization.
We will perform the critical reasoning network analysis to define the main NOC. (Figure 3).
Prioritized NOC of the DxEp.
Coping with problems: It is understood as the way in which the person manages losses in bodily functions or disabilities derived from diseases (Navarro & Bueno, 2015).
According to Nola Pender, nurse and author of the Health Promotion Model (HPM), expressed that behavior is motivated by the desire to achieve happiness and human potential. She is interested in creating a nursing model that provides answers about how people make decisions about their health care. It aims to illustrate the multifaceted nature of people in their interactions with the environment as they attempt to achieve a desired state of health; it emphasizes the connection between personal characteristics and the experiences, knowledge, beliefs, and situational aspects related to health behavior or the behavior a person wishes to achieve. In conclusion, problem coping is the way in which the person manages and accepts problems in order to achieve the solution.
(1302) Problem coping.
Definition: Personal actions to manage stressors that strain the individual›s resources.
Domain: Psychosocial health (III)
Class: Psychosocial adjustment (N)
In relation to the score plotted for the main NOC measurement for the DxEp, the assessment at the beginning of the nursing interventions was 2 points (Rarely demonstrated), and after the administration of nursing care, a target score of 4 points (Frequently demonstrated) is expected to be reached.
|
Table 1. Main NOC score for DxEp |
|||
|
NOC |
Initial Score |
Target Score |
Time |
|
(1302) Coping with problems |
2 |
4 |
12 |
|
Likert scale (1: Never demonstrated, 2: Rarely demonstrated, 3: Sometimes demonstrated, 4: Frequently demonstrated, 5: Always demonstrated). |
|||
Regarding the indicators plotted for the main NOC measurement for the DxEp, the assessment at the beginning of the nursing interventions was 2 points (Rarely demonstrated). After the administration of nursing care, a Target score of 4 points (Frequently demonstrated) is expected to be achieved.
|
Table 2. Main NOC indicator scores according to a Likert scale |
|||
|
Indicators |
Initial Score |
Target Score |
Time |
|
(130223) Obtains help from a health care professional |
2 |
4 |
12 |
|
(130205) Verbalizes acceptance of the situation |
2 |
4 |
12 |
|
(130220) Search for authoritative information about the diagnosis |
2 |
4 |
12 |
|
(130222) Search Accredited treatment information |
2 |
4 |
12 |
|
Likert scale (1: Never demonstrated, 2: Rarely demonstrated, 3: Sometimes demonstrated, 4: Frequently demonstrated, 5: Always demonstrated). |
|||
NIC Interventions for the DxEp NOC
Nursing interventions were identified using the NIC nursing intervention classification taxonomy of nursing interventions (Butcher Howard et al., 2018).
(5602) Teaching: Disease Process.
Definition: Helping the patient understand information related to a specific disease process.
Domain: 3. Behavioral
Class: S. Interventions to facilitate learning.
Activities:
· (560201) Review the patient’s knowledge of his or her condition.
· (560202) Provide information about available diagnostic measures as appropriate.
· (560203) Discuss therapy/treatment options.
· (560204) Instruct the patient on which signs and symptoms to report to the health care professional, as appropriate.
(6610) Risk identification.
Definition: Analysis of potential risk factors, determination of health risks, and prioritization of risk abatement strategies for an individual or group of people.
Domain 4: Safety
Class W: Risk Control
Activities:
· (661001) Review medical history and previous documents to determine evidence of current or previous medical and care diagnoses.
· (661002) Determine the availability and quality of resources (psychological, economic, educational level, family and other social resources, and community).
· (661003) Identify facility resources to help decrease risk factors.
· (661004) Determine compliance with medical and nursing treatments.
(5270) Emotional support.
Definition: Providing reassurance, acceptance, and encouragement in times of stress.
Domain 4: Behavioral
Class R: Coping assistance
Activities:
· (527001) Hugging or touching the patient to provide support.
· (527002) Helping the patient recognize feelings such as anxiety, anger, or sadness.
· (527003) Stay with the patient and provide feelings of reassurance during periods of heightened anxiety.
· (527004) Assist in decision-making.
With regard to the planned interventions on teaching about the disease process, identification of risks, and emotional support provided to the patient in a 12-hour shift, it is obtained that the planning is positive, observing a noticeable improvement in the patient, thus achieving stabilization of her symptomatology.
Classification of the Main Complication Risk (RC): Malignant Hypertension.
After performing the assessment and obtaining a nursing diagnosis, we proceed to make a follow-up plan for the patient using the NOC nursing outcome classification (Sue Moorhead et al.,2018) and NIC Nursing Interventions classification (Butcher Howard et al., 2018).
NOC outcome of the primary CR (RCp).
The NOC taxonomy responds to the outcomes we wish to achieve in the patient; 4-digit codes and 6-digit indicators are used.
The RCp Malignant hypertension responds to the following NOC: (1822) Knowledge: maternal health in preconception (0401) Circulatory status.
(0405) Cardiac tissue perfusion
(2112) Severity of hypertension
(0504) Renal function
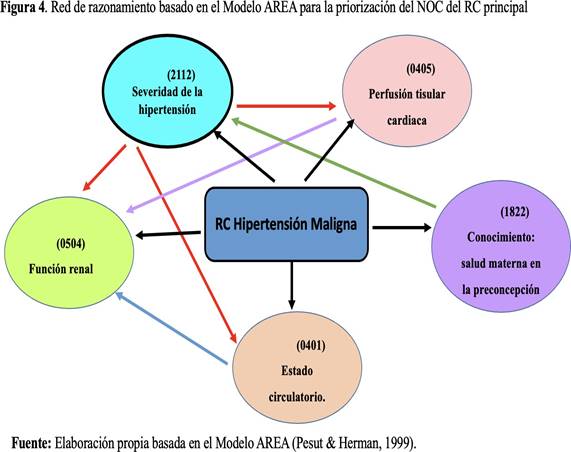
Prioritized NOC of major CR Malignant hypertension.
(2112) Severity of hypertension.
Definition: “Severity of signs and symptoms due to chronic blood pressure.” (Moorhead et al., 2018)
Domain: perceived health (V)
Class: symptomatology. (V)
|
Table 3. Main NOC score of the main CR |
||
|
NOC |
Initial Score |
Diana Score |
|
(2112) Severity of hypertension |
2 |
4 |
In relation to the main NOC score of the RCp, according to the Likert scale, an initial score of 2 points (substantial) was obtained for the patient’s assessment, with the goal of obtaining a target score of 4 points (Mild) after the nursing professional’s interventions during a 12-hour shift, giving a positive approach to the patient’s evolution.
|
Table 4. Scores of the main NOC indicators of the main CR according to Likert Scale |
|||
|
Indicators |
Initial Score |
Target Score |
Time |
|
(211207) Headache |
2 |
4 |
12 |
|
(211212) Tinnitus |
2 |
4 |
12 |
|
(211216) Increase of systolic P/A. |
2 |
4 |
12 |
|
(211217) Increased diastolic P/A. |
2 |
4 |
12 |
Interventions for risk of major complication (RCp).
Nursing interventions were considered in relation to RCp: Malignant hypertension, for which we used the NIC nursing intervention classification taxonomy (Butcher Howard et al., 2018).
(6200) Emergency care.
Definition: “Perform assessment and implement therapeutic measures in urgent situations” (Butcher et al., 2018).
Domain 4: safety: care that supports against harm Class U: crisis management.
Activities:
· (620001) Activate medical emergency system (620002). Monitor hypertensive vital signs.
· (620003) Provide reassurance and emotional support to the patient
· (620004) Assist with treatment by providing information about the potential situation
(6771) Electronic fetal monitoring: antepartum.
Definition: “Electronic assessment of fetal cardiac response to movement, external stimuli, or uterine contractions during antepartum testing” (Butcher et al., 2018).
Field 5: Family.
Class W: Caring for a new baby.
Activities:
· (677101) Review obstetric history, if available, to determine obstetric or medical risk factors pertaining to fetal status that would require antepartum testing to ascertain fetal status.
· (677102) Verify fetal and maternal heart rate prior to initiating electronic fetal monitoring.
· (677103) Interpret the electronic monitoring strip for long-term fetal heart rate variability and the presence of accelerations, decelerations, or spontaneous contractions.
· (677104) Observe the monitoring strip for the presence or absence of late decelerations.
· (677105) Report test results to the attending physician or midwife.
(4062) Circulatory care, arterial insufficiency.
Definition: “Improvement of arterial circulation” (Butcher et al., 2018).
Domain 2: Complex physiologic: Care that supports homeostatic regulation Class N: Control of tissue perfusion.
Activities:
· (406201) Perform a comprehensive assessment of peripheral circulation edema, capillary refill, color, and temperature.
· (406202) Evaluate edema and peripheral pulses
· (406203). Monitor water balance.
This last intervention was chosen since the main complication risk is “malignant hypertension” through the intervention of seizure management, being the drug used magnesium sulfate parenterally, executed in emergency care, thus avoiding the compromise of fetal distress.
EXECUTION
To implement the nursing interventions and activities, a 12-hour day shift is chosen; for this, the NIC Nursing Intervention Classification book was used (Butcher et al., 2018).
After administration of the main nursing interventions, in response to the DxEp NOC and the RCp NOC, change scores of +1 and +2 were obtained.
|
Table 5. Timeline of interventions/nursing activities in risk of maternal-fetal dyad disruption. |
||||||||
|
Date |
Interdependent and dependent activities |
Shifts |
||||||
|
8:30 |
10:00 |
12:00 |
14:00 |
16:00 |
18:00 |
20:30 |
||
|
9/9/2022 |
(00209) Risk of maternal-fetal dyad disruption. |
|||||||
|
Activities: |
X |
|
|
|
|
|
|
|
|
Teaching: Disease Process. |
X |
X |
|
|
|
|
|
|
|
Review the patient’s knowledge of his or her condition. |
X |
X |
|
|
|
|
|
|
|
Provide information about available diagnostic measures, as appropriate. |
|
X |
X |
|
|
|
|
|
|
Discuss therapy/treatment options. |
|
|
X |
X |
|
|
|
|
|
Instruct the patient as to which signs and symptoms to report to the healthcare notify the health care professional, as appropriate. |
|
|
|
X |
X |
|
|
|
|
Risk identification. |
X |
|
|
|
|
|
|
|
|
Review medical history and previous documents to determine evidence of current or prior determine evidence of current or previous medical and care diagnoses. |
X |
|
|
|
|
|
|
|
|
Determine the availability and quality of resources (psychological, economic, educational level, family and other social resources, and community). |
X |
X |
|
|
|
|
|
|
|
Identify the center’s resources to help decrease risk factors. |
X |
X |
|
|
|
|
|
|
|
Determine compliance with medical and nursing treatments. |
|
X |
X |
|
|
|
|
|
|
Emotional support |
X |
X |
X |
X |
X |
X |
X |
|
|
Hug or touch the patient to provide support. |
X |
|
|
|
|
|
|
|
|
Help the patient recognize feelings such as anxiety, anger or sadness. |
X |
X |
|
|
|
|
|
|
|
Staying with the patient and providing feelings of security during periods of heightened anxiety. |
X |
|
|
X |
|
|
|
|
|
Provide assistance in decision making. |
|
|
X |
|
|
|
|
|
|
|
(RCp) Malignant hypertension |
|||||||
|
Emergency Care |
X |
|
|
|
|
|
|
|
|
Activate the emergency medical system. |
X |
|
|
|
|
|
|
|
|
Monitor vital signs for hypertension. |
X |
|
X |
|
X |
|
X |
|
|
Provide reassurance and emotional support to the patient. |
X |
X |
X |
X |
X |
X |
X |
|
|
Assist with treatment by providing information about the situation. |
X |
|
|
|
|
|
|
|
|
Electronic fetal monitoring: before delivery |
X |
X |
X |
X |
X |
X |
X |
|
|
Review obstetrical history, if available, to determine obstetrical or medical risk factors concerning fetal status that require pre-delivery testing to verify fetal status |
X |
|
|
|
|
|
|
|
|
Check fetal and maternal heart rate before starting electronic fetal monitoring. |
X |
X |
X |
X |
X |
X |
X |
|
|
Interpret the electronic monitoring strip for long term fetal heart rate fetal heart rate, long-term variability and presence of accelerations, decelerations or spontaneous contractions. |
X |
X |
X |
X |
X |
X |
X |
|
|
Observe the monitoring strip for the presence or absence of late decelerations. |
X |
X |
X |
X |
X |
X |
X |
|
|
Communicate the test results to the responsible physician or midwife. |
X |
X |
X |
X |
X |
X |
X |
|
|
Circulatory care, arterial insufficiency |
X |
|
X |
|
X |
|
|
|
|
Perform comprehensive assessment of peripheral circulation edema, capillary refill, color and temperature. |
X |
|
X |
|
X |
|
|
|
|
Evaluate edema and peripheral pulses. |
X |
|
X |
|
X |
|
|
|
|
Monitor water balance. |
X |
|
|
X |
|
|
X |
|
EVALUATION
It was performed on the basis of the assessment of the pregnant woman’s condition at admission, compared with the results after the administration of the nursing interventions.
A follow-up period was established in the gynecology hospitalization service in the day shift; some progress was observed; however, continued care was needed. Nursing activities were evaluated based on a comparison of the patient’s health status and the effectiveness of planned outcomes.
Evaluation of the Outcome of the main Dx. E. main
(00209). Risk of disruption of the maternal-fetal dyad as evidenced by pregnancy
Complications due to multiple gestation.
Definition: Susceptible to disruption of the symbiotic mother-fetal relationship as a result of Comorbid or pregnancy-related conditions that may compromise health.
Domain 8: Sexuality
Class 3: Reproduction.
Analyzing the results obtained, the following is observed in relation to the indicators in Table 6; represented: (130223) Obtains help from a health professional, (130205) Verbalizes acceptance of the situation, (130220) Seeks accredited information about the diagnosis, (130222) Seeks accredited Information about the treatment, the patient started with a score of 2 (Rarely demonstrated) and reached a score of 3 (Sometimes demonstrated) in 12 hours, in the course of this time she was able to be attended by a multidisciplinary team, where she was able to verbalize about the situation that affects her, managing to find a diagnosis about her disease process and obtain an adequate treatment to stabilize her altered health patterns and achieve the recovery of the mother and the conservation of the gestation through the care applied.
|
Table 6. Scores of the main diagnostic indicators according to Likert Scale |
||||
|
Indicators |
Initial Score |
Diana Score |
Score achieved |
Time |
|
(130223) Obtains help from a health care health professional |
2 |
4 |
3 |
12 |
|
(130205) Verbalizes acceptance of the situation |
2 |
4 |
3 |
12 |
|
(130220) Seeks reputable information about the diagnosis |
2 |
4 |
3 |
12 |
|
(130222) Search for accredited treatment information |
2 |
4 |
|
12 |
(1302) Coping with problems.
Definition: Personal actions to manage stressors that strain the individual’s resources.
Domain: Psychosocial health (III)
Class: Psychosocial coping (N)
The interventions were carried out achieving the proposed target score, the initial score being 2 points, after a period of 12 hours in the gynecology hospitalization service. A score of 4 points according to the Likert scale was achieved, reaching compliance with problem coping.
|
Table 7. Main NOC score for DxEp |
||||
|
NOC |
Initial Score |
Diana Score |
Score achieved |
Time |
|
(1302) Coping with problems |
2 |
5 |
4 |
12 |
|
(Likert scale: 1. Serious, 2. Substantial, 3. Moderate, 4. Slight, 5. None) |
||||
Evaluation of the main complication risk score.
The programmed nursing interventions were carried out, obtaining the proposed target score, the initial score being 2 points, after a period of 12 hours in the hospital. A score of 3 points was achieved according to the Likert scale, achieving moderate management of the severity of hypertension in the pregnant woman.
|
Table 8. Main NOC score of the main CR |
|||
|
NOC |
Initial Score |
Diana Score |
Score Achieved |
|
(2112) Severity of hypertension |
2 |
5 |
4 |
Observing the results obtained, the following is observed: in relation to the indicators in Table 9, represented: (21207) headache, (211212) tinnitus, (211216) increased systolic P/A, (211217) increased diastolic P/A, the patient started with a score of 2 (substantial) and reached a score of 4 (mild) on the Likert scale in 12 hours, achieving a good score in the stabilization of the symptomatology presented by means of the care applied by the multidisciplinary health care team.
Table 9. Scoring of the main NOC indicators of the main CR according to Likert Scale |
||||
|
Indicators |
Initial Score |
Diana Score |
Score achieved |
Time |
|
(211207) Headache |
2 |
5 |
4 |
12 |
|
(211212) Tinnitus |
2 |
5 |
4 |
12 |
|
(211216) Increase of systolic P/A. |
2 |
5 |
4 |
12 |
|
(211217) Increased diastolic P/A. |
2 |
5 |
4 |
12 |
(Likert scale: 1. Serious, 2. Substantial, 3. Moderate, 4. Slight, 5. None) |
||||
DISCUSSION
The patient in the present study was admitted to the gynecology hospitalization service, presenting a temperature of 38. 7 °C, headache, tinnitus, abdominopelvic pain, lower limb edema, and P/A 190/110mm Hg, with medical diagnosis: preeclampsia and twin gestation of 30 weeks due to FUR and CR of malignant hypertension as a consequence of the disorder in the third trimester of pregnancy; for which, she is in the gynecology hospitalization service after being referred from the emergency area for timely care to avoid damage.
After reviewing the literature, numerous studies have been obtained showing that nursing care is essential, comprehensive quality care, and is key to preventing cerebrovascular, cardiovascular, and renal diseases. In affirming the above, there is scientific evidence that the nursing professional has a key role in prenatal care for the timely detection, prevention, diagnosis, and treatment that can attenuate the factors that can condition maternal and perinatal morbidity and mortality. (Guarnizo et. al., 2019).
The elaboration and execution of the nursing care plan as an instrument to establish and document the actual situation of the patient, the expected outcomes, interventions, and evaluation allow constant monitoring to improve the weaknesses found. Nursing care is both autonomous and collaborative for the delivery of services in person-centered care (PAHO, 2022).
Psychophysiological changes during pregnancy are often accompanied by different emotions, which occur throughout pregnancy, such as mood swings, irritability, fear, and anxiety. For this reason, a pregnant woman is considered emotionally unstable and, therefore, needs to be treated humanely and feel satisfied with her care by a qualified multidisciplinary team of medical professionals. Likewise, we consider the mother’s family as another major component of the comprehensive care provided and of the nursing intervention that should be directed to the partner and family, who are also directly concerned with maternal health problems. To help improve (Maset, 2021).
In the case presented, the informant was the patient; data collection and assessment were carried out through assessment instruments, relying on interviews and observation, as well as other sources of data collection.
Nursing interventions are based on the theories of Hildegard E. Peplau, who seeks to highlight the psychological tasks that develop from the nurse-patient relationship, depending on the nurse’s ability to recognize the difficulties posed by relationships with their patients and the ability to help them resolve their difficulties so that they can develop new faculties for coping with problems (Martinez Esquivel, 2020).
This theory, in relation to the patient’s situation after the diagnosis of Risk of alteration of the maternal-fetal dyad in the patient with twin gestation of 30 weeks, oriented us to improve the coping of problems by improving the nurse-patient relationship. Likewise, our care was oriented in the theory of “Humanized Care” by Jean Watson, decreasing the risk of dehumanization in patient care and rescuing the human, spiritual, and transpersonal aspects during the nursing care of the pregnant patient (Gaona Castillo, 2021).
The risk of alteration of the maternal-fetal dyad occurs as a consequence of pregnancy complications such as hypertension and due to a deficit of knowledge on the part of the mother, in the face of which the nursing professional participates in the timely treatment, avoiding maternal vascular lesions, such as hepatic compromise, renal damage, kidney damage, etc. (Gaona Castillo, 2021) hepatic compromise, renal damage, and consequently fetal compromise (Department of Obstetrics, UC de Chile, 2020).
Malignant hypertensive CR manifests with a high risk of seizures and risk of fetal compromise (Tango, 2020). Timely intervention with nursing actions plays a very important
The timely intervention with nursing actions plays a very important role as they are aimed at the prevention of this maternal and perinatal complication problem, with the purpose of contributing to the reduction of maternal morbidity and establishing technical criteria for the prevention, diagnosis, treatment, and control of preeclampsia.
To conclude, as health professionals, we have the responsibility to perform a good assessment and, through our timely care, reduce the risks of complications in the maternal-fetal binomial. After the nursing care provided to the patient at a critical moment, we were able to assess a favorable evolution compared to the initial phase of care in the gynecology hospitalization service.
LIMITATIONS
· The limitations encountered in the development of the case study in the twin pregnant woman with preeclampsia were:
· Limited time for monitoring and care to those who were only attended during a 12-hour shift in the gynecology service.
· It was not possible to continue with the care in the following days due to interference with the working hours of the nursing professionals.
· When applying nursing care, we had the limitation of finding the appropriate diagnoses and interventions for the patient’s pathology because the NOC and NIC do not include the diagnosis of preeclampsia.
· At the same time, due to the situation of the COVID-19 pandemic, the conditions for family access to information were limited since visits were restricted in the institution.
CONCLUSIONS
Preeclampsia is a hypertensive disorder that can occur during pregnancy from 20 weeks of gestation and becomes a serious condition representing a major danger to the mother-fetus binomial. In Peru (2020-2021), maternal deaths represent 21,4 % (2020) and 15,8 % (2021). (MINSA, 2022); this indicator allows us to measure the impact of health policy on the provision of maternal health services.
The EAP was applied, developing the nursing care plan, according to the NANDA I. taxonomy, NOC, NIC, and Lynda Carpenito’s bifocal model for a patient with twin gestation, preeclampsia and risk of complication: malignant hypertension, in order to promote professional practice with a creative approach based on human responses to specific situations.
The assessment by functional patterns was based on the theoretical framework, on the nursing theory of Hildegard Peplau and Jean Watson, which helped to identify the nursing diagnosis of risk of alteration of the maternal-fetal dyad and problem of collaboration in the prenatal stage: gestational hypertension and risk of complication: malignant hypertension.
The risk factors of the patient with twin gestation and preeclampsia were identified and described, considering situations, personal characteristics, and diseases that have hindered the patient’s ability to continue with the pregnancy and project us toward recovery due to her vulnerability to the risk of complication: malignant hypertension.
Ninety percent of the activities of the nursing care plan were fulfilled, where the actions were protocolized based on the patient’s needs and monitored to consolidate the evaluation and define the improvement of the patient’s interventions through participatory work with the multidisciplinary team for the solution of the collaborative problem.
Nursing care, as a basic and primordial tool, strengthened the autonomy and empowerment of the nurse in the care of the patient with preeclampsia; for the achievement of the objectives in the evolution of the disease process.
Through the care plan, the proposed objectives were achieved by prioritizing the main nursing diagnosis to provide timely and quality care, improving maternal-fetal health status.