Comparative study between physiological healing vs. the use of platelet-rich fibrin at the time of bone and gingival tissue healing in lower third molar surgeries. Bibliographic Review
Estudio comparativo entre la cicatrización fisiológica vs el uso de fibrina rica en plaquetas al momento de la cicatrización de tejido óseo y gingival en cirugías de terceros molares inferiores. Revisión Bibliográfica
Mónica Alexandra Acosta Vargas1 * ![]() , Ronald
Medardo Gómez Coba1 *
, Ronald
Medardo Gómez Coba1 * ![]() , Jhoseline
Melissa Pérez Villacrés1 *
, Jhoseline
Melissa Pérez Villacrés1 * ![]() , Mónica
Sofía Pallo Sarabia1 *
, Mónica
Sofía Pallo Sarabia1 * ![]()
1Universidad Regional Autónoma de Los Andes, Sede Ambato. Ecuador.
![]()
Submitted: 16-12-2023 Revised: 17-03-2024 Accepted: 18-06-2024 Published: 19-06-2024
How to Cite: Acosta Vargas MA, Gómez Coba RM, Pérez Villacrés JM, Pallo Sarabia MS. Comparative study between physiological healing vs. the use of platelet-rich fibrin at the time of bone and gingival tissue healing in lower third molar surgeries. Bibliographic Review. Interamerican Journal of Health Sciences. 2024; 4:122. https://doi.org/10.59471/ijhsc2024122
ABSTRACT
Introduction: the extraction of retained third molars can present surgical complications, causing various alterations to the patient, such as pain after the intervention, inflammation during the next 24 to 72 hours, jaw pain, among others.
Objective: to compare the effectiveness of physiological healing vs. the use of platelet-rich fibrin at the time of bone and gingival tissue healing in lower third molar surgeries by means of a bibliographic review and thereby identify the properties and factors that promote healing. cicatrization.
Method: qualitative and descriptive bibliographic review, based on the PRISMA (2020) method, inclusion and exclusion criteria were used, in addition to search strings created using MeSH terms and Boolean operators to search the databases, PubMed, ScienceDirect, and Scielo.
Results: a total of 12 scientific articles with valid information for the investigation were obtained. It was determined that platelet-rich fibrin is better than physiological healing for bone and gingival tissue healing in lower third mandibular surgeries.
Conclusions: it is concluded that the application of Platelet Rich Fibrin (PRF) promotes the healing process of the tissues and reduces discomfort such as pain, inflammation and bleeding after mandibular third molar surgery, although advanced Platelet Rich Fibrin variants (A-PRF) and leukocyte- and platelet-rich fibrin (L-PRF) are more efficient than simple PRF.
KEYWORDS
Healing, Platelet-Rich Fibrin, Third Molars, Bone Tissue, Gingival Tissue.
RESUMEN
Introducción: la extracción de terceros molares puede generar complicaciones quirúrgicas provocando diversas alteraciones al paciente, como dolor tras la intervención, inflamación durante las siguientes 24 a 72 horas, dolor mandibular entre otras.
Objetivo: comparar la efectividad que tiene la cicatrización fisiológica vs el uso de fibrina rica en plaquetas al momento de la cicatrización de tejido óseo y gingival en cirugías de terceros molares inferiores mediante revisión bibliográfica y con ello identificar cuáles son las propiedades y factores que promueven la cicatrización
Método: revisión bibliográfica de tipo cualitativo y descriptivo, fundamentada en el método PRISMA (2020), se utilizaron criterios de inclusión e exclusión, además de cadenas de búsqueda creadas mediante términos MeSH y operadores boléanos para realizar la búsqueda en las bases de datos, PubMed, ScienceDirect y SciElo.
Resultados: se obtuvieron un total de 12 artículos científicos con información válida para la investigación. Se determinó que la fibrina rica en plaquetas es mejor que la cicatrización fisiológica, para la cicatrización de tejido óseo y gingival en cirugías de terceros mandibulares inferiores.
Conclusiones: se concluye que la aplicación de Fibrina rica en plaquetas (PRF) promueve el proceso de cicatrización de los tejidos y reduce las molestias como dolor, inflamación y sangrado después de una cirugía de terceros molares mandibulares, aunque las variantes Fibrina rica en plaquetas avanzada (A- PRF) y Fibrina rica en leucocitos y plaquetas (L-PRF) son más eficientes que la PRF simple.
PALABRAS CLAVE
Cicatrización, Fibrina Rica en Plaquetas, Terceros Molares, Tejido Óseo, Tejido Gingival.
INTRODUCTION
The extraction of third molars can generate surgical complications causing various alterations to the patient, such as pain after the intervention, inflammation during the following 24 to 72 hours, and mandibular pain, among others.(1)
At the same time, third molar extraction affects the periodontal condition of the gums and the mandibular second molar. The incidence of periodontitis in the bone and gingival tissue of the third molar is 23% after the third molar surgery.(2) However, due to the lack of obvious short-term subjective symptoms, practitioners are often unaware of the effects of third molar extraction on periodontal health; therefore, affected gingival tissue is rarely treated.(3)
On the other hand, gingival tissue damage has a high prevalence in the population that has undergone third molar extraction and is considered a complex condition.(4) Therefore, the preparation of surgically injured tissues for healing is an important aspect of any surgical procedure.(5)
The healing of the alveolar cavity, or healing after tooth extraction, involves remodeling of the bone and soft tissues, and the most important dimensional changes occur in the first three months.(6)
Regarding the healing of the cavity after extraction, there are two types of healing in dentistry: healing by first intention and healing by second intention. (1) Sutures achieve healing by first intention and the use of chemical materials, and healing by second intention al, so-called physiological healing, is achieved by spontaneous closure of the surgical wound. (7) Physiological healing is a fundamental response of the organism, in which the satisfactory restoration of tissue integrity is conditioned. Healing is not an isolated phenomenon but a process regulated by biochemical factors, and changes in tissue structure ultimately determine scar formation.(8)
On the other hand, there are many ways to improve hard and soft tissue healing and maintain tissue volume after tooth extraction.(9) Many studies have demonstrated the benefits of using techniques such as grafts, growth factors, and absorbable or non-absorbable membranes for alveolar protection.(10)
Among the resorbable elements are bioactive materials of autologous origin, such as platelet concentrates rich in growth factors, which have been used as an alternative to periodontal therapy.(8) In this regard, autologous platelet concentrates, including platelet-rich fibrin (PRF) and platelet-rich plasma (PRP), have, in recent years, gained immense popularity in tissue engineering.(11)
In the same context, platelet-rich fibrin (PRF), a second-generation autologous growth factor obtained by centrifugation from non-anticoagulated autologous blood, was originally developed in France as a therapeutic alternative to PRP to overcome many of its limitations. FRP is easy to manufacture, non-toxic, biocompatible with living tissue, promotes healing, is believed to be associated with early organization of effective bone mass and bone volume percentage, and is relatively inexpensive.(6) In conjunction, platelet concentrates have been used for several years to improve postoperative outcomes after extraction of impacted third molars. These concentrates are obtained from human blood and are centrifuged by various methods to obtain extraction of third molars. They can generate surgical complications causing various alterations to the patient, such as pain after the intervention, inflammation during the following 24 to 72 hours, and mandibular pain, among others.(1)
At the same time, third molar extraction affects the periodontal condition of the gums and the mandibular second molar. The incidence of periodontitis in the bone and gingival tissue of the third molar is 23% after the third molar surgery.(2) However, due to the lack of obvious short-term subjective symptoms, practitioners are often unaware of the effects of third molar extraction on periodontal health; therefore, affected gingival tissue is rarely treated.(3)
On the other hand, gingival tissue damage has a high prevalence in the population that has undergone third molar extraction and is considered a complex condition.(4) Therefore, the preparation of surgically injured tissues for healing is an important aspect of any surgical procedure.(5)
The healing of the alveolar cavity, or healing after tooth extraction, involves remodeling of the bone and soft tissues, and the most important dimensional changes occur in the first three months.(6)
Regarding the healing of the cavity after extraction, there are two types of healing in dentistry: healing by first intention and healing by second intention. (1) Sutures achieve healing by first intention and the use of chemical materials, and healing by second intention al, so-called physiological healing, is achieved by spontaneous closure of the surgical wound.(7) Physiological healing is a fundamental response of the organism, in which the satisfactory restoration of tissue integrity is conditioned. Healing is not an isolated phenomenon but a process regulated by biochemical factors, and changes in tissue structure ultimately determine scar formation.(8)
On the other hand, there are many ways to improve hard and soft tissue healing and maintain tissue volume after tooth extraction.(9) Many studies have demonstrated the benefits of using techniques such as grafts, growth factors, and absorbable or non-absorbable membranes for alveolar protection.(10)
Among the resorbable elements are bioactive materials of autologous origin, such as platelet concentrates rich in growth factors, which have been used as an alternative to periodontal therapy.(8) In this regard, autologous platelet concentrates, including platelet-rich fibrin (PRF) and platelet-rich plasma (PRP), have, in recent years, gained immense popularity in tissue engineering. (11)
In the same context, platelet-rich fibrin (PRF), a second-generation autologous growth factor obtained by centrifugation from non-anticoagulated autologous blood, was originally developed in France as a therapeutic alternative to PRP to overcome many of its limitations. FRP is easy to manufacture, non-toxic, biocompatible with living tissue, promotes healing, is believed to be associated with early organization of effective bone mass and bone volume percentage, and is relatively inexpensive.(6) In conjunction, platelet concentrates have been used for several years to improve postoperative outcomes after extraction of impacted third molars. These concentrates are obtained from human blood and are centrifuged by various methods to obtain them.(12)
However, the ideal method for the management of bone and gingival tissue healing in lower third molar surgeries is still a matter of controversy, so the present study aimed to compare the effectiveness of physiological healing vs. the use of platelet-rich fibrin at the time of bone and gingival tissue healing in lower third molar surgeries through literature review and thus identify which are the properties and factors that promote healing in them.(12)
However, the ideal method for the management of bone and gingival tissue healing in lower third molar surgeries is still a matter of controversy, so the present study aimed to compare the effectiveness of physiological healing vs. the use of platelet-rich fibrin at the time of bone and gingival tissue healing in lower third molar surgeries through literature review and thus identify which are the properties and factors that promote healing.(13)
METHOD
This article had a method based on qualitative analysis generated from a literature review, where a collection and review of literature in scientific databases was carried out with the purpose of acquiring relevant information that contributes to achieving the research objective.
Types of research
Type of research according to the approach
The research approach was qualitative because it focused on studying the effectiveness of the use of platelet-rich fibrin for the healing of bone and gingival tissues after lower third molar surgeries. A literature review was executed consisting of the collection of scientific literature published in the period 2018 to 2023, with information relevant to the topic of study.
Type of research according to the objective and scope.
Due to its objective, the present research was of a descriptive type, seeking to describe how the use of platelet-rich fibrin after lower third molar surgeries influences healing; for this purpose, a scientific data collection was performed that allowed drawing objective conclusions on the study topic. In addition, we sought to describe in detail the factors that affect physiological and platelet-rich fibrin-assisted healing at the time of bone and gingival tissue healing.
Techniques and Instruments
The present research used the literature review technique of original scientific articles published from January 2018 to June 2023. As search tools, scientific databases such as PubMed, SciELO and ScienceDirect were used where to perform a correct search, and advanced search strings were created consisting of keywords (MeSH) and Boolean terms (AND, OR, NOT). At the same time, in order to simplify the search, the following eligibility criteria were established:
Inclusion Criteria
· Articles were included with the keywords established in the present work.
· Studies conducted in humans were included.
· Research published in the period 2018-2023 was included.
· Scientific articles published in Spanish, English and Portuguese were included.
· Studies analyzing the effectiveness of physiological healing at the time of bone and gingival tissue healing in lower third molar surgeries were included.
· We included studies analyzing the effectiveness of platelet-rich fibrin at the time of bone and gingival tissue healing in third molar surgeries.
Exclusion Criteria
· Study of articles analyzing the use of platelet-rich fibrin in areas other than dentistry.
· Study of articles analyzing the efficacy of physiological healing in lesions of body parts other than the mouth.
· Animal studies.
· Review studies (literature review or systematic review).
· Articles older than the established period.
Methods to be used
For the design of this article, the search criteria established in the PRISMA 2020 Statement: an updated guide for the publication of systematic reviews in the health area (13) were used as a guide. This method is composed of a series of steps to collect and analyze the most relevant information on a given topic, either updating existing knowledge or creating new knowledge. Table 1 summarizes the methodology used to carry out the article.
|
Table 1. Summary of PRISMA methodology |
|
|
Section |
Item |
|
Eligibility Criteria |
Inclusion and exclusion criteria. |
|
Sources of information |
PubMed, Scielo, ScienceDirect. |
|
Search strings |
(((Cicatrization) AND (gingival tissue)) AND (Platelet Rich Fibrin)) AND (third molar surgeries). ((Cicatrization) AND (gingival tissue)) AND (third molar surgeries) (third molar surgeries) AND (Platelet Rich Fibrin) |
|
Selection process |
Discarding of duplicates. Title reading, summary reading. Relevant data and information will be chosen by reading each article in its entirety. |
|
Data collection process |
Excel was used to generate a flow diagram. Subsequently, a data collection template was created. |
|
MeSH Terms |
Cicatrization, Platelet Rich Fibrin, osseous tissue, gingival tissue, third molar surgeries, third molar surgeries) |
|
List of data |
Efficacy of physiological healing and scarring with the use of platelet-rich fibrin for bone and gum tissue healing. |
|
Synthesis methods |
The results of the studies included in the literature review are presented in tables for better understanding. |
RESULTS
Through the use of search strings in the previously mentioned databases, a total of 277 articles were identified, of which 36 duplicate articles were eliminated after reading the title. Then, by reading the summary, 47 articles were eliminated for being studies that analyze healing in surgeries of other dental pieces, 54 for only analyzing third molar surgeries, 42 for analyzing platelet-rich fibrin in other surgical processes, in addition, articles were eliminated after the complete reading for not having significant contributions 24, for analyzing the perception of people about platelet-rich fibrin 36 and for analyzing platelet-rich fibrin without taking into account third molar surgeries 23. Also, two articles were excluded for not presenting solid results and 1 for needing a consistent population, leaving a total of 12 scientific articles. The process can be seen in figure 1.
|
Table 2. Results by search engine and search string |
||
|
Search engine |
Chain |
Result |
|
PubMEd |
(third molar surgeries) AND (Platelet Rich Fibrin) |
47 |
|
ScienceDirect |
(third molar surgeries) AND (Platelet Rich Fibrin) |
219 |
|
Scielo |
(third molar surgeries) AND (Platelet Rich Fibrin) |
11 |
|
Total |
277 |
|
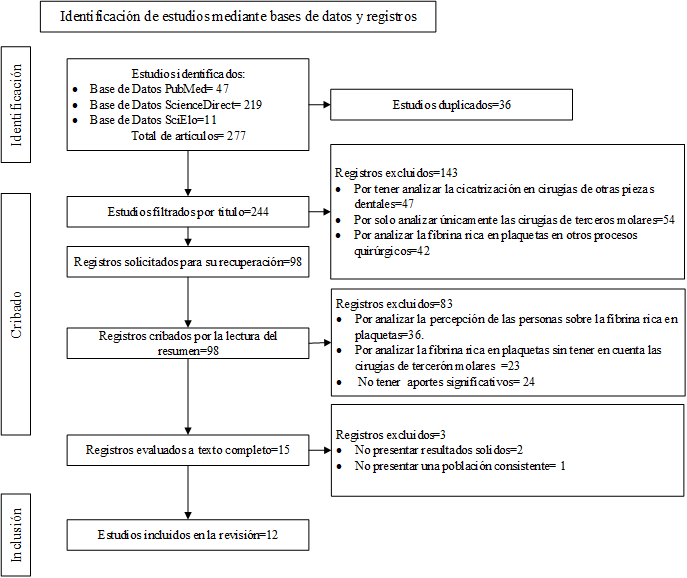
Figure 1. Flow chart for item selection according to the PRISMA guide (2020).
The results obtained from the scientific articles are presented in table 3.
|
Table 3. Results of scientific studies |
||||||
|
Nº |
Author |
Population |
Study design |
Intervention performed |
Results |
Conclusions |
|
1 |
Afat et al.(14) |
60 patients aged 18 to 30 years. 22 men and 38 women |
Prospective, randomized, double-blind, controlled study. Third molar surgery (M3) |
Application of leukocyte- and platelet-rich fibrin (L-PRF) in 20 patients. Combination of L-PRF and hyaluronic acid (HA) (n = 20). Control group nothing was applied (n = 20). |
The mean mucosal healing scores at days 7, 14 and 21 for both the L-PRF and L-PRF + HA groups were significantly better than those of the control group. There were no cases of alveolar osteitis or postoperative wound infection in the L-PRF and L-PRF + HA groups, whereas in the control group it was 1:20. |
The results of this study suggest that L-PRF alone and when combined with HA may be an effective way to improve soft tissue healing and could be used to prevent postoperative alveolar osteitis and infection after surgery. |
|
2 |
Zahid et al.(15) |
10 patients |
Randomized, double-blind clinical trial. Surgical extractions of impacted third molars. |
Advanced platelet-rich fibrin (A-PRF) was placed on one side of the mandible, while the other side received no intervention. |
There were no significant differences in pocket depth (PD), clinical attachment level (CAL) and gingival recession (GR) between the two groups at any time point, although the data obtained slightly favored A-PRF. A statistically significant reduction in pain and swelling was observed in the A-PRF group compared to controls (p < 0,05). |
The findings of this study demonstrate that A-PRF is a potential biomaterial to decrease the severity of pain and swelling after third molar surgery. |
|
3 |
Shruthi et al.(16) |
44 patients aged 18 to 40 years |
Randomized, double-blind clinical trial. Third molar surgery |
Primary closure in the control group (Group 22) PRF was placed in the study group (22 patients). |
The application of PRF in the study group decreases the severity of immediate postoperative sequelae such as pain, swelling and trismus compared to the control group. |
Treatment outcomes and postoperative sequelae were better in the PRF group compared to another control group at days 1, 3, and 7 postoperatively. |
|
4 |
Ritto et al.(17) |
17 patients |
Prospective, double-blind, split-mouth study.
Mandibular third molar extraction |
On one side, the alveolus was mainly sutured (control side). On the other side, L-PRF was inserted before suturing. |
The application of L-PRF improved bone density, which was higher in the test group (p=0,007). There was no statistical difference related to pain or soft tissue between groups (p>0,05). There was evidence of improved bone healing in response to L-PRF. |
To better understand the effect of L-PRF, more clinical trials with larger samples are needed. |
|
5 |
Caymaz et al.(18) |
27 patients 15 women and 12 men between 18 and 26 years old. |
Randomized, double-blind clinical trial. Mandibular third molar surgery. |
For the first and second groups, A-PRF and L-PRF were applied respectively. |
The L-PRF group’s visual analog scale pain scores on day 1 (P < 0,05), day 2 and day 3 and total values (P < 0,01); number of analgesics on days 2 (P < 0,01) and 3; and their total values (P < 0,05) were significantly higher than those of the A-PRF group. |
The use of A-PRF after mandibular third molar extraction significantly reduces postoperative pain and patients need to take analgesics in the A-PRF group compared to the L-PRF group. |
|
6 |
Torul et al.(19) |
75 patients |
Randomized, double-blind clinical trial. Mandibular third molar surgery. |
Three groups A-PRF (n = 25), concentrated growth factors CGF (n = 25) and control (n = 25). |
The outcome variables trismus, pain and analgesic consumption showed no significant differences between groups (P>0,05). |
Based on the results of this study, it can be concluded that A-PRF and CGF seem to have no positive effects on pain, edema and trismus after third molar surgery. |
|
7 |
Njokanma et al.(20) |
90 patients |
Prospective study. Surgical extraction of mandibular third molars |
One PRF group (intervention group) One group without PRF (control group) |
The percentage of neoformed bone region (RNFB%) was not significantly higher in the PRF group compared to the non-PRF group. In the PRF group, the middle third had the highest bone formation. |
Placement of PRF in extraction sockets increased alveolar bone regeneration. However, this finding was not statistically significant. |
|
8 |
Alam et al.(21) |
40 patients |
Prospective study.Mandibular third molar extraction. |
PRF group (n = 20)PRF with HA group(n = 20) |
Pain and swelling were lower in the PRF with HA group compared to the PRF group.Soft tissue healing was better in the PRF with HA group compared to the PRF group. |
PRF a mitogenic promoter together with a bone graft forms a scaffold, promotes early healing, thus creating benefits for the patient and is also economical. |
9 |
Riaz et al.(22) |
10 patients (3 males, 7 females; 18-35 years) |
Randomized, double-blind clinical trial.Mandibular third molar extraction. |
A-PRF and PRF were placed on the right side for 5 patients in each group.In both groups, the left side of the patients was taken as the control group. |
The A-PRF group recorded a marked improvement in pain (P = 0,063), swelling (P = 0,001) and mouth opening (P = 0,013) compared to the PRF and control group. |
The advanced PRF group showed decreased swelling, pain and increased mouth opening compared to the PRF and control group. |
|
10 |
Yüce et al.(23) |
40 patients |
Randomized clinical trial.Mandibular third molar extraction. |
Group I (control; saline only); Group II (use of A-PRF +). |
With respect to pain, the application of A-PRF + demonstrated a rapid and continuous reduction in pain intensity. Statistically, epithelial and hard tissue healing rates were significantly faster in the A-PRF + application group (P: 0,000, P < 0,05). |
The results show that A-PRF+ could represent an improved and accelerated therapeutic development for hard and soft tissue healing in the treatment of alveolar osteitis that is also effective in reducing pain. |
|
11 |
Sybila et al.(24) |
25 patients |
Randomized, double-blind clinical trial.Mandibular third molar extraction |
The randomly assigned test side received PRF and the other side acted as control. |
There was a statistically significant improvement in the signs and symptoms of pain, tenderness, edema and sensitivity of patients with the use of PRF. There was a statistically significant improvement in sulcus bleed (SBI), plaque index and probing depths. PRF use did not influence CALs and bone height. |
PRF is a very viable and useful biomaterial for soft tissue healing and alleviation of patient symptoms, however, it does not aid in hard tissue healing with respect to cortical bone. |
|
12 |
Travezán et al.(6) |
51 patients |
Single Blind, Randomized, Crossover, Controlled Clinical Trial Mandibular third molar extraction |
Group A (control) was left with a blood clot for normal healing. Group B (experimental) was administered PRF |
When comparing both groups in soft tissue healing, it was found that the group with PRF presented a better recovery, with a statistically significant difference at 7 and 14 days after surgery (p<0,05). |
FRP has a positive effect on alveolar soft tissue healing after atraumatic exodontia, independent of sex and age. |
|
Note: PRF=Platelet Rich Fibrin; A-PRF=Advanced Platelet Rich Fibrin; L-PRF=Leukocyte and Platelet Rich Fibrin; HA=hyaluronic acid; PD=pouch depth; CAL=clinical attachment level; GR=gum recession; SBI=Sulcus Bleeding; SBI=Sulcus Bleeding. |
||||||
DISCUSSION
Through the literature review, it was possible to compare the effectiveness of physiological healing vs. the use of platelet-rich fibrin (PRF) at the time of bone and gingival tissue healing in lower third molar surgeries. It was identified that the use of PRF after a surgical process in mandibular third molars promotes the healing process, as demonstrated in their studies by Afat et al. (14), Shruthi et al. (16), Njokanma et al. (20), Alam et al. (21), Sybila et al. (24), Travezán et al. (6)
Regarding the benefits of the use of PRF after the extraction process of mandibular third molars, it can be mentioned that it helps to reduce discomfort, such as pain and inflammation, demonstrated by Shruthi et al. (16), Alam et al. (21) Sybila et al. (24) while Njokanma et al. (20), determined that the placement of PRF in extraction sockets increased alveolar bone regeneration.
With regard to PRF types, A-PRF was also identified as excellent for improving healing and reducing discomfort after mandibular third molar surgery, according to Zahid and Nadershah (15), Riaz et al. (22), Caymaz and Uyanik. (18) At the same time, Yüce and Kömerik (23) found that A-PRF application showed faster epithelial and hard tissue healing rates. However, Torul et al. (19) in their research did not find positive results regarding the use of A-PRF in the reduction of pain, trismus and analgesic consumption.
On the other hand, with respect to L-PRF, it was determined that it helps to improve bone density. Meticone Ritto et al. (2019) (17) found that the application of L-PRF improved bone density in patients, while Afat et al. (14) identified that L-PRF alone and when combined with HA can be an effective way to improve soft tissue healing.
On the other hand, when comparing the different types of PRF, it was determined that A-PRF is superior to L-PRF and traditional PRF in improving healing, in accordance with the results obtained by Caymaz and Uyanik (18) and Riaz et al. (22)
Furthermore, with regard to periodontal parameters, Zahid and Nadershah (15) determined that the application of A-PRF after surgical extractions of impacted third molars presents better results in pocket depth (PD), clinical attachment level (CAL) and gingival recession (GR) with respect to physiological healing alone, while Sybila et al. (2020) (24) determined that the use of PRF does not influence CAL.
CONCLUSIONS
The application of platelet-rich fibrin (PRF) promotes the tissue healing process. It reduces discomfort such as pain, inflammation, and bleeding after mandibular third molar surgery. However, the variants Advanced Platelet Rich Fibrin (A-PRF) and Leukocyte and Platelet Rich Fibrin (L-PRF) are more efficient than simple PRF, so when possible, the use of PRF can be chosen.
It is essential to have prior training, supplies, and equipment to perform venipuncture.
It is necessary to carry out more studies with a larger population and thus obtain more precise results on the use of PRF since most of the studies analyzed were carried out with a population of less than 100 people.
REFERENCIAS BIBLIOGRÁFICAS
1. Guzmán G, Paltas M, Benenaula J, Núñez K, Simbaña D. Cicatrización de tejido óseo y gingival en cirugías de terceros morales inferiores. Estudio comparativo entre el uso de fibrina rica en plaquetas versus cicatrización fisiológica. Rev Odontológica Mex [Internet]. 2017;21(2):114–20. Available from: https://www.scielo.org.mx/pdf/rom/v21n2/1870-199X-rom-21-02-00114.pdf
2. Castagna V, Pardo A, Lanaro L, Signoriello A, Albanese M. Periodontal Healing after Lower Third Molars Extraction: A Clinical Evaluation of Different Flap Designs. Healthc (Basel, Switzerland) [Internet]. 2022 Aug;10(8):1–13. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9408120/
3. Zhang Y, Chen X, Zhou Z, Hao Y, Li H, Cheng Y, et al. Effects of impacted lower third molar extraction on periodontal tissue of the adjacent second molar. Ther Clin Risk Manag [Internet]. 2021;17(1):235–47. Available from: https://www.dovepress.com/getfile.php?fileID=67863
4. Salgado Á, Salgado Á, Arriba L. Nuevas tendencias en regeneración tisular: fibrina rica en plaquetas y leucocitos. Rev Esp Cir Oral y Maxilofac [Internet]. 2017;39(2):91–8. Available from: https://scielo.isciii.es/pdf/maxi/v39n2/1130-0558-maxi-39-02-00091.pdf
5. Hanif M, Sheikh MA. Efficacy of platelet rich plasma (PRP) on mouth opening and pain after surgical extraction of mandibular third molars. J Oral Med Oral Surg [Internet]. 2021;27(1):3–9. Available from: https://www.jomos.org/articles/mbcb/pdf/2021/01/mbcb200021.pdf
6. Travezán M, Aguirre A, Arbildo H. Effect of the Platelet-Rich Fibrin on the Healing of the Soft Tissues of Sockets after Atraumatic Exodontics. A Single-Blind Cross-Randomized Controlled Clinical Trial. Int J Odontostomat [Internet]. 2021;15(1):240–7. Available from: https://www.scielo.cl/pdf/ijodontos/v15n1/0718-381X-ijodontos-15-01-240.pdf
7. Alencastro S, Ordóñez C. Complications in the extraction of impacted , and retained third molars . Literature Review . Rev Odontol Vital [Internet]. 2023;1(38):26–33. Available from: https://www.scielo.sa.cr/pdf/odov/n38/en_1659-0775-odov-38-17.pdf
8. López E, Pascual A. Fibrina rica en plaquetas en la cicatrización de los tejidos periodontales. Odontol Sanmarquina [Internet]. 2020;23(1):43–50. Available from: https://docs.bvsalud.org/biblioref/2020/03/1053510/17506-texto-del-articulo-60950-1-10-20200221.pdf
9. Esra E. The Effect of Platelet-Rich Fibrin and Titanium Prepared Platelet-Rich Fibrin on Early Soft Tissue Healing of Extraction Sites. Cumhur Dent J [Internet]. 2018;21(4):304–10. Available from: http://cdj.cumhuriyet.edu.tr/en/download/article-file/617841
10. Makki A, Alsulami A, Almatrafi A, Sindi M, Sembawa S. The Effectiveness of Advanced Platelet-Rich Fibrin in comparison with Leukocyte-Platelet-Rich Fibrin on Outcome after Dentoalveolar Surgery. Int J Dent [Internet]. 2021;21(1):1–9. Available from: https://downloads.hindawi.com/journals/ijd/2021/6686857.pdf
11. Sharma A, Ingole S, Deshpande M, Ranadive P, Sharma S, Kazi N, et al. Influence of platelet-rich fibrin on wound healing and bone regeneration after tooth extraction: A clinical and radiographic study. J oral Biol craniofacial Res [Internet]. 2020;10(4):385–90. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7393389/
12. Cruz C, Castro Y. Resultados de los concentrados plaquetarios en la regeneración ósea guiada. Rev Cuba Investig Biomed [Internet]. 2020;39(2):1–20. Available from: http://scielo.sld.cu/pdf/ibi/v39n2/1561-3011-ibi-39-02-e515.pdf
13. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. Declaración PRISMA 2020: una guía actualizada para la publicación de revisiones sistemáticas. Rev Española Cardiol. 2021;74(9):790–9.
14. Afat I, Akdoğan E, Gönül O. Effects of leukocyte- and platelet-rich fibrin alone and combined with hyaluronic acid on early soft tissue healing after surgical extraction of impacted mandibular third molars: A prospective clinical study. J Craniomaxillofac Surg [Internet]. 2019 Feb;47(2):280–6. Available from: https://pubmed.ncbi.nlm.nih.gov/30579747/
15. Zahid T, Nadershah M. Effect of Advanced Platelet-rich Fibrin on Wound Healing after Third Molar Extraction: A Split-mouth Randomized Double-blind Study. J Contemp Dent Pract [Internet]. 2019 Oct;20(10):1164–70. Available from: https://pubmed.ncbi.nlm.nih.gov/31883251/
16. Shruthi T, Shetty A, Akash K, Ahmed F, Shetty N, Singarapu R. Evaluation of effects of platelet-rich fibrin on treatment outcomes after impacted mandibular third molar surgery: A randomized controlled clinical study. Natl J Maxillofac Surg [Internet]. 2022 Aug;13(1):46–51. Available from: https://pubmed.ncbi.nlm.nih.gov/36393932/
17. Ritto F, Pimentel T, Canellas J, Junger B, Cruz M, Medeiros P. Randomized double-blind clinical trial evaluation of bone healing after third molar surgery with the use of leukocyte- and platelet-rich fibrin. Int J Oral Maxillofac Surg [Internet]. 2019 Aug;48(8):1088–93. Available from: https://pubmed.ncbi.nlm.nih.gov/30910410/
18. Caymaz M, Uyanik L. Comparison of the effect of advanced platelet-rich fibrin and leukocyte- and platelet-rich fibrin on outcomes after removal of impacted mandibular third molar: A randomized split-mouth study. Niger J Clin Pract [Internet]. 2019 Apr;22(4):546–52. Available from: https://pubmed.ncbi.nlm.nih.gov/30975961/
19. Torul D, Omezli M, Kahveci K. Evaluation of the effects of concentrated growth factors or advanced platelet rich-fibrin on postoperative pain, edema, and trismus following lower third molar removal: A randomized controlled clinical trial. J Stomatol oral Maxillofac Surg [Internet]. 2020 Dec;121(6):646–51. Available from: https://pubmed.ncbi.nlm.nih.gov/32068167/
20. Njokanma A, Fatusi O, Ogundipe O, Arije O, Akomolafe A, Kuye O. Does platelet-rich fibrin increase bone regeneration in mandibular third molar extraction sockets? J Korean Assoc Oral Maxillofac Surg [Internet]. 2022 Dec;48(6):371–81. Available from: https://pubmed.ncbi.nlm.nih.gov/36579909/
21. Alam S, Khare G, Arun Kumar K. A Comparative Study of Platelet-Rich Fibrin and Platelet-Rich Fibrin with Hydroxyapatite to Promote Healing of Impacted Mandibular Third Molar Socket. J Maxillofac Oral Surg [Internet]. 2022 Jun;21(2):608–15. Available from: https://pubmed.ncbi.nlm.nih.gov/35712405/
22. Riaz R, Radhakrishnan M, Perumal J. Comparative Study of the Efficacy of Advanced Platelet-rich Fibrin and Standard Platelet-rich Fibrin in Mandibular Third Molar Surgery. J Pharm Bioallied Sci [Internet]. 2022 Jul;14(1):781–7. Available from: https://pubmed.ncbi.nlm.nih.gov/36110692/
23. Yüce E, Kömerik N. Potential effects of advanced platelet rich fibrin as a wound-healing accelerator in the management of alveolar osteitis: A randomized clinical trial. Niger J Clin Pract [Internet]. 2019 Sep;22(9):1189–95. Available from: https://pubmed.ncbi.nlm.nih.gov/31489852/
24. Sybila D, Sawai M, Faisal M, Singh S, Jain V. Platelet-Rich Fibrin for Hard- and Soft-Tissue Healing in Mandibular Third Molar Extraction Socket. Ann Maxillofac Surg [Internet]. 2020;10(1):102–7. Available from: https://pubmed.ncbi.nlm.nih.gov/32855924/T
FINANCING
There is no funding for this work.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Mónica Alexandra Acosta Vargas, Ronald Medardo Gómez Coba, Jhoseline Melissa Pérez Villacrés, Mónica Sofía Pallo Sarabia.
Research: Mónica Alexandra Acosta Vargas, Ronald Medardo Gómez Coba, Jhoseline Melissa Pérez Villacrés, Mónica Sofía Pallo Sarabia.
Methodology: Mónica Alexandra Acosta Vargas, Ronald Medardo Gómez Coba, Jhoseline Melissa Pérez Villacrés, Mónica Sofía Pallo Sarabia.
Project administration: Mónica Alexandra Acosta Vargas, Ronald Medardo Gómez Coba, Jhoseline Melissa Pérez Villacrés, Mónica Sofía Pallo Sarabia.
Original drafting and editing: Mónica Alexandra Acosta Vargas, Ronald Medardo Gómez Coba, Jhoseline Melissa Pérez Villacrés, Mónica Sofía Pallo Sarabia.
Writing-revision and editing: Mónica Alexandra Acosta Vargas, Ronald Medardo Gómez Coba, Jhoseline Melissa Pérez Villacrés, Mónica Sofía Pallo Sarabia.